3
WTCS Learning Objectives
- Apply the rules of medical language to build, analyze, spell, pronounce, abbreviate, and define terms as they relate to the integumentary system
- Identify meanings of key word components of the integumentary system
- Categorize diagnostic, therapeutic, procedural or anatomic terms related to the integumentary system
- Use terms related to the integumentary system
- Use terms related to the diseases and disorders of the integumentary system
Integumentary System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Integumentary System.
Introduction to the Integumentary System
The integumentary system refers to the skin and its accessory structures. In the adult human body, the skin makes up about 16 percent of body weight and covers an area of 16-21 ft2.
In fact, the skin and accessory structures are the largest organ system in the human body. The skin protects your inner organs and it is in need of daily care and protection to maintain its health.
Watch this video:
Media 3.1. The science of skin – Emma Bryce [Video]. Copyright 2018 by Ted-Ed.
Practice integumentary system medical terms.
Anatomy (Structures) of the Integumentary System
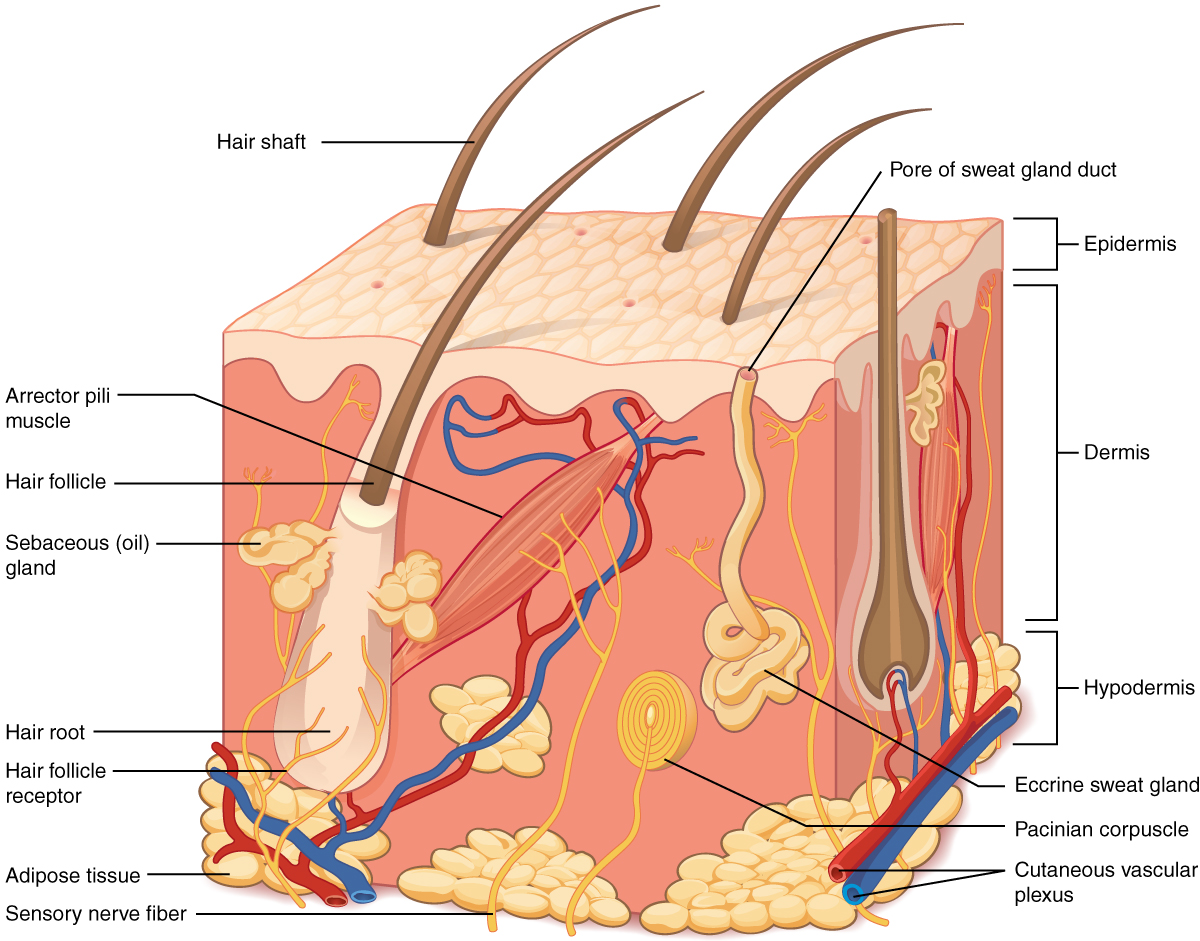
The skin and its accessory structures make up the integumentary system, which provides the body with overall protection. The skin is made of multiple layers of cells and tissues, which are held to underlying structures by connective tissue. The deeper layer of skin is well vascularized. It also has numerous sensory, and autonomic and sympathetic nerve fibers ensuring communication to and from the brain.
The skin is composed of two main layers:
- The epidermis
- The dermis
- Beneath the dermis lies the hypodermis
Concept Check
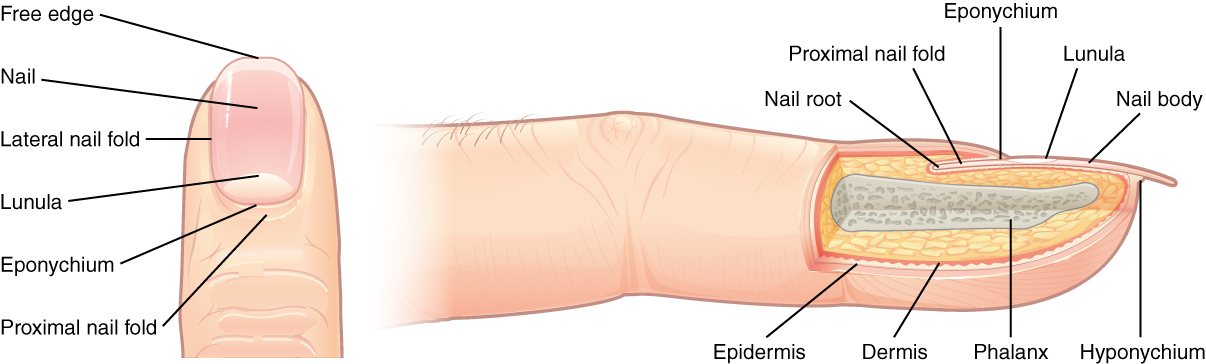
- On the diagram above find the two layers of the skin; epidermis and dermis.
- The literal breakdown for hypodermis is below the dermis. On the diagram above where can you locate it?
- Can you find a hair follicle, hair root and hair shaft?
- Keep reading to find out what the arrector pilli muscle does when you are frightened.
Epidermis
The epidermis is composed of keratinized, stratified squamous epithelium. It is made of four or five layers of epithelial cells, depending on its location in the body. It is avascular.
The cells in all of the layers except the stratum basale are called keratinocytes. Keratin is an intracellular fibrous protein that gives hair, nails, and skin their hardness and water-resistant properties. The keratinocytes in the stratum corneum are dead and regularly slough away, being replaced by cells from the deeper layers.
Dermis
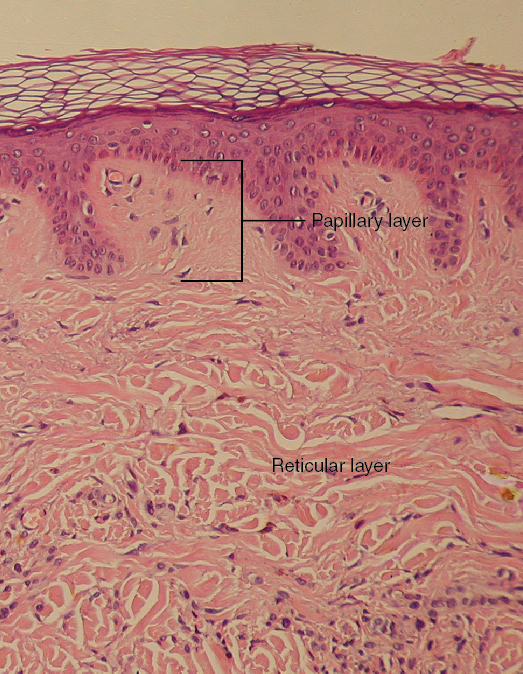
Papillary Layer
The papillary layer is made of loose, areolar connective tissue, which means the collagen and elastin fibers of this layer form a loose mesh. This superficial layer of the dermis projects into the stratum basale of the epidermis to form finger-like dermal papillae (see Figure 3.2). Within the papillary layer are fibroblasts, a small number adipocytes, and an abundance of small blood vessels. In addition, the papillary layer contains phagocytes, that help fight bacteria or other infections that have breached the skin. This layer also contains lymphatic capillaries, nerve fibers, and Meissner corpuscles.
Reticular Layer
Underlying the papillary layer is the much thicker reticular layer, composed of dense, irregular connective tissue. This layer is well vascularized and has a rich sensory and sympathetic nerve supply. The reticular layer appears reticulated due to a tight meshwork of fibers. Elastin fibers provide some elasticity to the skin, enabling movement. Collagen fibers provide structure and tensile strength, with strands of collagen extending into both the papillary layer and the hypodermis. In addition, collagen binds water to keep the skin hydrated. Collagen injections and Retin-A creams help restore skin turgor by either introducing collagen externally or stimulating blood flow and repair of the dermis, respectively.
Hypodermis
The hypodermis serves to connect the skin to the underlying fascia of the bones and muscles. It is not strictly a part of the skin, although the border between the hypodermis and dermis can be difficult to distinguish. The hypodermis consists of well-vascularized, loose, areolar connective tissue and [pb_glossary id="1697"]adipose[/pb_glossary] tissue, which functions as a mode of fat storage and provides insulation and cushioning for the integument.
Practice labeling the layers of the skin.
Physiology (Function) of the Integumentary System
The skin and accessory structures perform a variety of essential functions, such as protecting the body from invasion by microorganisms, chemicals, and other environmental factors; preventing dehydration; acting as a sensory organ; modulating body temperature and electrolyte balance; and synthesizing vitamin D. The underlying hypodermis has important roles in storing fats, forming a “cushion” over underlying structures, and providing insulation from cold temperatures.
Protection
The skin protects the body from wind, water, and UV sunlight. It acts as a protective barrier against water loss and it also is the first line of defense against abrasive activity such as grit, microbes, or harmful chemicals. Sweat excreted from sweat glands deters microbes from over-colonizing the skin surface.
Sensory Function
The skin acts as a sense organ because the epidermis, dermis, and the hypodermis contain specialized sensory nerve structures that detect touch, surface temperature, and pain. These receptors are more concentrated on the tips of the fingers, which are most sensitive to touch, especially the Meissner corpuscle, which responds to light touch, and the Pacinian corpuscle , which responds to vibration. Merkel cells, seen scattered in the stratum basale, are also touch receptors. In addition to these specialized receptors, there are sensory nerves connected to each hair follicle, pain and temperature receptors scattered throughout the skin, and motor nerves innervate the arrector pili muscles and glands. This rich innervation helps us sense our environment and react accordingly,
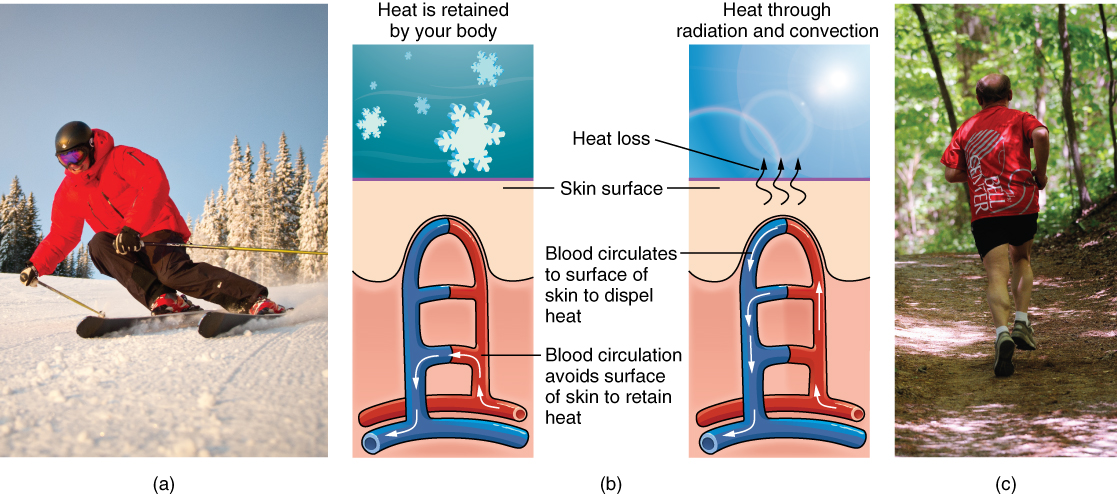
Thermoregulation
The integumentary system helps regulate body temperature through its tight association with the sympathetic nervous system. The sympathetic nervous system is continuously monitoring body temperature and initiating appropriate motor responses.
- When the body becomes warm sweat glands, accessory structures to the skin, secrete water, salt, and other substances to cool the body.
- Even when the body does not appear to be noticeably sweating, approximately 500 mL of sweat are secreted a day.
- If the body becomes excessively warm due to high temperatures, vigorous activity, or a combination of the two, sweat glands will be stimulated by the sympathetic nervous system to produce large amounts of sweat.
- When the sweat evaporates from the skin surface, the body is cooled as body heat is dissipated.
- In addition to sweating, arterioles in the dermis dilate so that excess heat carried by the blood can dissipate through the skin and into the surrounding environment.
- This accounts for the skin redness that many people experience when exercising.
- When body temperatures drop, the arterioles constrict to minimize heat loss, particularly in the ends of the digits and tip of the nose.
- This reduced circulation can result in the skin taking on a whitish hue.
- Although the temperature of the skin drops as a result, passive heat loss is prevented, and internal organs and structures remain warm.
- If the temperature of the skin drops too much (such as environmental temperatures below freezing), the conservation of body core heat can result frostbite .
Concept Check
Can you describe the thermoregulation process between the integumentary system and the sympathetic system?
- When body temperature is too warm.
- When body temperature is too cold.
Vitamin D Synthesis
The epidermal layer of human skin synthesizes Vitamin D when exposed to UV radiation. In the presence of sunlight, a form of Vitamin D3 called cholecalciferol is synthesized from a derivative of the steroid cholesterol in the skin. The liver converts cholecalciferol to calcidiol, which is then converted to calcitriol (the active chemical form of the vitamin) in the kidneys.
- Vitamin D is essential for normal absorption of calcium and phosphorous, which are required for healthy bones.
- The absence of sun exposure can lead to a lack of vitamin D in the body, in children this can cause rickets. Vitamin D deficiency in elderly individuals may lead to osteomalacia.
- In present day society, Vitamin D is added as a supplement to many foods, including milk and orange juice, compensating for the need for sun exposure. In addition to its essential role in bone health, Vitamin D is essential for general immunity against bacterial, viral, and fungal infections.
Watch this video:
Media 3.2. The Integumentary System, Part 2 – Skin Deeper: Crash Course A&P #7 [Online video]. Copyright 2015 by CrashCourse.Media 3.2. The Integumentary System, Part 2 – Skin Deeper: Crash Course A&P #7 [Online video]. Copyright 2015 by CrashCourse.
Accessory Structures
Accessory structures of the skin include hair, nails, sweat glands, and sebaceous glands. These structures embryologically originate from the epidermis and can extend down through the dermis into the hypodermis.
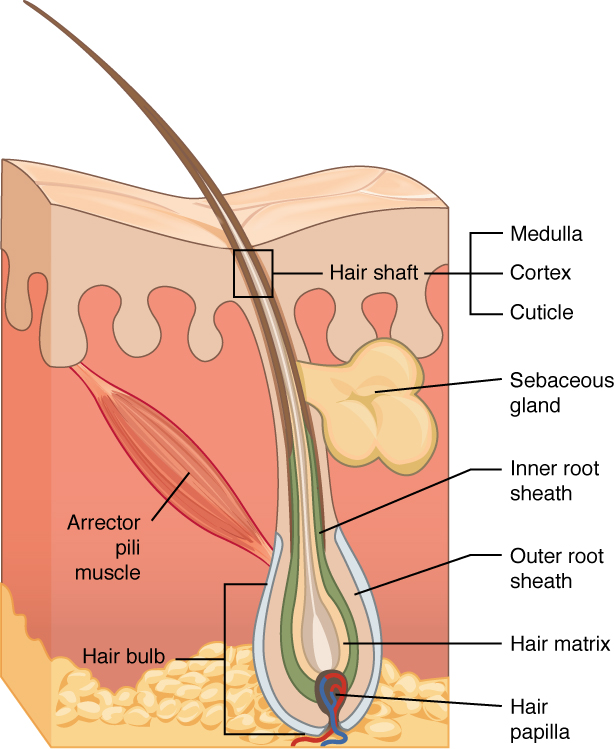
Hair
Hair is a keratinous filament growing out of the epidermis. It is primarily made of dead, keratinized cells. Strands of hair originate in an epidermal penetration of the dermis called the hair follicle. The hair shaft is the part of the hair not anchored to the follicle, and much of this is exposed at the skin’s surface. The rest of the hair, which is anchored in the follicle, lies below the surface of the skin and is referred to as the hair root. The hair root ends deep in the dermis at the hair bulb, and includes a layer of mitotically active basal cells called the hair matrix. The hair bulb surrounds the hair papilla, which is made of connective tissue and contains blood capillaries and nerve endings from the dermis (see Figure 3.4).
Hair Function
Hair serves a variety of functions, including protection, sensory input, thermoregulation, and communication. For example:
- Hair on the head protects the skull from the sun.
- Hair in the nose and ears, and around the eyes (eyelashes) defends the body by trapping and excluding dust particles that may contain allergens and microbes.
- Hair of the eyebrows prevents sweat and other particles from dripping into and bothering the eyes.
Hair also has a sensory function due to sensory innervation by a hair root plexus surrounding the base of each hair follicle. Hair is extremely sensitive to air movement or other disturbances in the environment, much more so than the skin surface. This feature is also useful for the detection of the presence of insects or other potentially damaging substances on the skin surface.
Each hair root is connected to a smooth muscle called the arrector pili that contracts in response to nerve signals from the sympathetic nervous system, making the external hair shaft “stand up.” The primary purpose for this is to trap a layer of air to add insulation. This is visible in humans as goose bumps and even more obvious in animals, such as when a frightened cat raises its fur. Of course, this is much more obvious in organisms with a heavier coat than most humans, such as dogs and cats.
Hair Growth, Loss and Color
Hair grows and is eventually shed and replaced by new hair. Hair typically grows at the rate of 0.3 mm per day. On average, 50 hairs are lost and replaced per day. Hair loss occurs if there is more hair shed than what is replaced and can happen due to hormonal or dietary changes. Hair loss can also result from the aging process, or the influence of hormones. Similar to the skin, hair gets its color from the pigment melanin, produced by melanocytes in the hair papilla. Different hair color results from differences in the type of melanin. As a person ages, the melanin production decreases, and hair tends to lose its color and becomes gray and/or white.
Nails
The nail bed is a specialized structure of the epidermis that is found at the tips of our fingers and toes. The nail body is formed on the nail bed, and protects the tips of our fingers and toes as they are the farthest extremities and the parts of the body that experience the maximum mechanical stress (see Figure 3.5). The nail body forms a back-support for picking up small objects with the fingers. The nail body is composed of densely packed dead keratinocytes.
The epidermis in this part of the body has evolved a specialized structure upon which nails can form. The nail body forms at the nail root, which has a matrix of proliferating cells from the stratum basale that enables the nail to grow continuously. The lateral nail fold overlaps the nail on the sides, helping to anchor the nail body. The nail fold that meets the proximal end of the nail body forms the nail cuticle, also called the eponychium.
The nail bed is rich in blood vessels, making it appear pink, except at the base, where a thick layer of epithelium over the nail matrix forms a crescent-shaped region called the lunula (the “little moon”). The area beneath the free edge of the nail, furthest from the cuticle, is called the hyponychium. It consists of a thickened layer of stratum corneum.
Sweat Glands
Sudoriferous Glands
When the body becomes warm, sudoriferous glands produce sweat to cool the body. Sweat glands develop from epidermal projections into the dermis and are classified as merocrine glands; that is, the secretions are excreted by exocytosis through a duct without affecting the cells of the gland. There are two types of sweat glands, each secreting slightly different products.
An eccrine sweat gland is type of gland that produces a hypotonic sweat for thermoregulation as described previously. These glands are found all over the skin’s surface, but are especially abundant on the palms of the hand, the soles of the feet, and the forehead (Figure 3.6). They are coiled glands lying deep in the dermis, with the duct rising up to a pore on the skin surface, where the sweat is released. This type of sweat, released by exocytosis, is hypotonic and composed mostly of water, with some salt, antibodies, traces of metabolic waste, and dermicidin, an antimicrobial peptide. Eccrine glands are a primary component of thermoregulation in humans and thus help to maintain homeostasis .
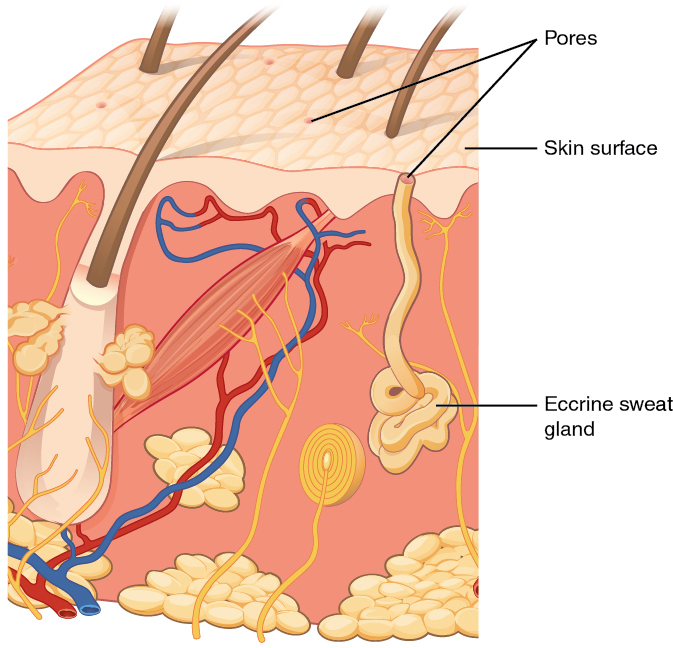
An apocrine sweat gland is usually associated with hair follicles in densely hairy areas, such as armpits and genital regions. Apocrine sweat glands are larger than eccrine sweat glands and lie deeper in the dermis, sometimes even reaching the hypodermis, with the duct normally emptying into the hair follicle. In addition to water and salts, apocrine sweat includes organic compounds that make the sweat thicker and subject to bacterial decomposition and subsequent smell. The release of this sweat is under both nervous and hormonal control, and plays a role in the poorly understood human pheromone response. Most commercial antiperspirants use an aluminum-based compound as their primary active ingredient to stop sweat. When the antiperspirant enters the sweat gland duct, the aluminum-based compounds precipitate due to a change in pH and form a physical block in the duct, which prevents sweat from coming out of the pore.
Sebaceous Glands
A sebaceous gland is a type of oil gland that is found all over the body and helps to lubricate and waterproof the skin and hair. Most sebaceous glands are associated with hair follicles. They generate and excrete sebum, a mixture of lipids, onto the skin surface, thereby naturally lubricating the dry and dead layer of keratinized cells of the stratum corneum, keeping it pliable. The fatty acids of sebum also have antibacterial properties, and prevent water loss from the skin in low-humidity environments. The secretion of sebum is stimulated by hormones, many of which do not become active until puberty. Thus, sebaceous glands are relatively inactive during childhood.
Words not Easily Broken into Word Parts
Common Integumentary System Abbreviations
Many terms and phrases related to the integumentary system are abbreviated. Learn these common abbreviations by expanding the list below.
Changes Due to Aging
All systems in the body accumulate subtle and some not-so-subtle changes as a person ages. Among these changes are reductions in cell division, metabolic activity, blood circulation, hormonal levels, and muscle strength (see Figure 3.7). In the skin, these changes are reflected in decreased mitosis in the stratum basale, leading to a thinner epidermis. The dermis, which is responsible for the elasticity and resilience of the skin, exhibits a reduced ability to regenerate, which leads to slower wound healing. The hypodermis, with its fat stores, loses structure due to the reduction and redistribution of fat, which in turn contributes to the thinning and sagging of skin.

The accessory structures also have lowered activity, generating thinner hair and nails, and reduced amounts of sebum and sweat. A reduced sweating ability can cause some elderly to be intolerant to extreme heat. Other cells in the skin, such as melanocytes and dendritic cells, also become less active, leading to a paler skin tone and lowered immunity. Wrinkling of the skin occurs due to breakdown of its structure, which results from decreased collagen and elastin production in the dermis, weakening of muscles lying under the skin, and the inability of the skin to retain adequate moisture.
Disease and Disorders
The integumentary system is susceptible to a variety of diseases, disorders, and injuries. These range from annoying but relatively benign bacterial or fungal infections that are categorized as disorders, to skin cancer and severe burns, which can be fatal. In this section, you will learn several of the most common skin conditions.
One of the most talked about diseases is skin cancer. Most cancers are identified by the organ or tissue in which the cancer originates. One common form of cancer is skin cancer.
In general, cancers result from an accumulation of DNA mutations. These mutations can result in cell populations that do not die when they should and uncontrolled cell proliferation that leads to tumors. Although many tumors are benign, some metastasize. Cancers are characterized by their ability to metastasize.
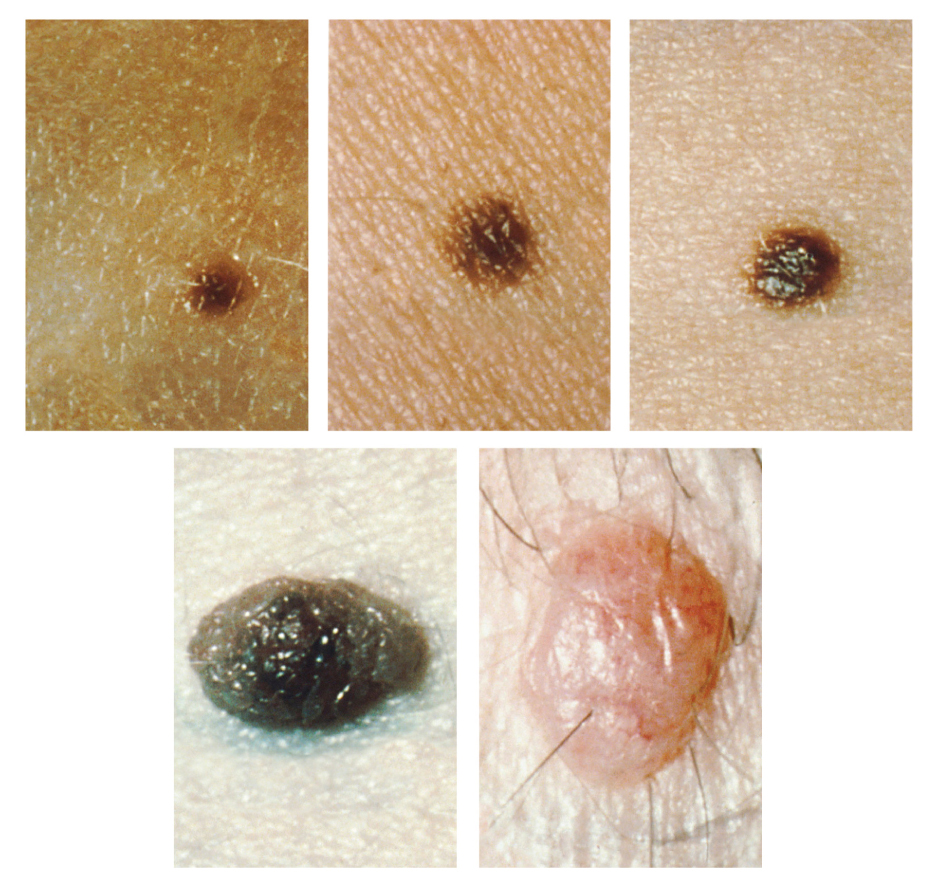
Sun Damage
It requires about 10 days after initial sun exposure for melanin synthesis to peak, which is why pale-skinned individuals tend to suffer sunburns of the epidermis initially. Dark-skinned individuals can also get sunburns, but are more protected than are pale-skinned individuals. Too much sun exposure can eventually lead to wrinkling due to the destruction of the cellular structure of the skin, and in severe cases, can cause sufficient DNA damage to result in skin cancer. When there is an irregular accumulation of melanocytes in the skin, freckles appear. Moles are larger masses of melanocytes, and although most are benign, they should be monitored for changes that might indicate the presence of cancer (see Figure 3.8).
Basal Cell Carcinoma (BCC)
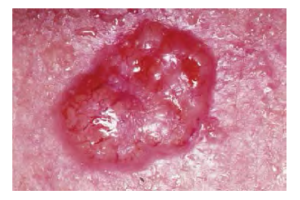
Basal cell carcinoma is a form of cancer that affects the mitotically active stem cells in the stratum basale of the epidermis. It is the most common of all cancers that occur in the United States and is frequently found on the head, neck, arms, and back, which are are as that are most susceptible to long-term sun exposure. Although UV rays are the main culprit, exposure to other agents, such as radiation and arsenic, can also lead to this type of cancer. Wounds on the skin due to open sores, tattoos, burns, etc. may be predisposing factors. Basal cell carcinomas start in the stratum basale and usually spread along this boundary. At some point, they begin to grow toward the surface and become an uneven patch, bump, growth, or scar on the skin surface (see Figure 3.9). Like most cancers, basal cell carcinomas respond best to treatment when caught early. Treatment options include surgery, freezing (cryosurgery), and topical ointments.
Squamous Cell Carcinoma (SCC)

Squamous cell carcinoma is a cancer that affects the keratinocytes of the stratum spinosum and presents as lesions commonly found on the scalp, ears, and hands (see Figure 3.10). It is the second most common skin cancer. The American Cancer Society reports that two of 10 skin cancers are squamous cell carcinomas, and it is more aggressive than basal cell carcinoma. If not removed, these carcinomas can metastasize. Surgery and radiation are used to cure squamous cell carcinoma.
Melanoma
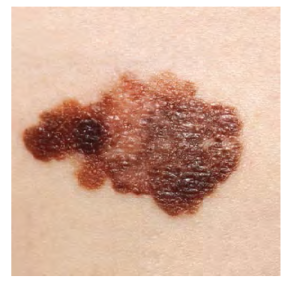
A melanoma is a cancer characterized by the uncontrolled growth of melanocytes, the pigment-producing cells in the epidermis. Typically, a melanoma develops from a mole. It is the most fatal of all skin cancers, as it is highly metastatic and can be difficult to detect before it has spread to other organs. Melanomas usually appear as asymmetrical brown and black patches with uneven borders and a raised surface (see Figure 3.11). Treatment typically involves surgical excision and immunotherapy.
ABCDE for Early Diagnosis
Doctors often give their patients the following ABCDE mnemonic to help with the diagnosis of early-stage melanoma (see Fig 3.12). If you observe a mole on your body displaying these signs, consult a doctor.
- Asymmetry – the two sides are not symmetrical
- Borders – the edges are irregular in shape
- Color – the color is varied shades of brown or black
- Diameter – it is larger than a pencil eraser
- Evolving – its shape has changed
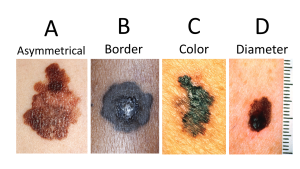
Some specialists cite the following additional signs for the most serious form, nodular melanoma:
Elevated – it is raised on the skin surface
Firm – it feels hard to the touch
Growing – it is getting larger
Albinism
Albinism is a genetic disorder that affects (completely or partially) the coloring of skin, hair, and eyes. This is primarily due to the inability of melanocytes to produce melanin. Individuals with albinism tend to appear white or very pale due to the lack of melanin in their skin and hair. Recall that melanin helps protect the skin from the harmful effects of UV radiation. Individuals with albinism tend to need more protection from UV radiation, as they are more prone to sunburns and skin cancer. They also tend to be more sensitive to light and have vision problems due to the lack of pigmentation on the retinal wall (Betts, et al., 2021)
Treatment of this disorder usually involves addressing the symptoms, such as limiting UV light exposure to the skin and eyes. In vitiligo, the melanocytes in certain areas lose their ability to produce melanin, possibly due to an autoimmune reaction. This leads to a loss of color in patches (see Figure 3.13). Neither albinism nor vitiligo directly affects the lifespan of an individual (Betts, et al., 2021)

Changes in Skin Coloration
Other changes in the appearance of skin coloration can be indicative of diseases associated with other body systems.
- Liver disease or liver cancer can cause the accumulation of bile and the yellow pigment bilirubin, leading to xanthoderma or jaundice.
- Tumors of the pituitary gland can result in the secretion of large amounts of melanocyte-stimulating hormone (MSH), which results in a darkening of the skin.
- Addison’s disease can stimulate the release of excess amounts of adrenocorticotropic hormone (ACTH), which can give the skin a deep bronze color
- A sudden drop in oxygenation can affect skin color, causing the skin to initially turn ashen (white).
- A prolonged reduction in oxygen levels, dark red deoxyhemoglobin becomes dominant in the blood, making the skin appear blue, a condition referred to as cyanosis. This happens when the oxygen supply is restricted, as when someone is experiencing difficulty in breathing because of asthma or a heart attack. However, in these cases the effect on skin color has nothing do with the skin’s pigmentation (Betts, et al., 2021)
Skin Disorders
Two common skin disorders are eczema and acne. Eczema is an inflammatory condition and occurs in individuals of all ages. Acne involves the clogging of pores, which can lead to infection and inflammation, and is often seen in adolescents. Other disorders, include seborrheic dermatitis (on the scalp), psoriasis, fungal infections, cold sores, impetigo, scabies, hives, and warts (Betts, et al., 2021).
Eczema

Eczema is an allergic reaction that manifests as dry, itchy patches of skin that resemble rashes (see Figure 3.14). It may be accompanied by swelling of the skin, flaking, and in severe cases, bleeding. Symptoms are usually managed with moisturizers, corticosteroid creams, and immunosuppressants (Betts, et al., 2021).
Acne
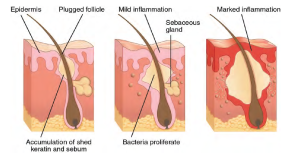
Acne is a skin disturbance that typically occurs on areas of the skin that are rich in sebaceous glands (face and back). It is most common along with the onset of puberty due to associated hormonal changes, but can also occur in infants and continue into adulthood. Hormones, such as androgens, stimulate the release of sebum. An overproduction and accumulation of sebum along with keratin can block hair follicles. This plug is initially white. The sebum, when oxidized by exposure to air, turns black. Acne results from infection by acne-causing bacteria (Propionibacterium and Staphylococcus), which can lead to redness and potential scarring due to the natural wound healing process (see Figure 3.15) (Betts, et al., 2021).
Ringworm
Tinea or dermatophytosis is often referred to as ringworm. Ringworm presents as a circular rash that is itchy and red and can be found on various parts of the body. It is referred to by the location that it is found:
-
- Tinea Pedis – feet or commonly referred to as athlete’s feet
- Tinea Capitis – scalp
- Tinea barbae – beard
- Tinea manuum – hands
- Tinea unguium – Toenails and fingernails also called onychomycosis
- Tinea corporis – Body parts such as arms and legs (Center for Disease Control and Prevention, 2018a)
To learn more about ringworm, visit the Center for Disease Control and Prevention’s web page on fungal infections.
Psoriasis
Psoriasis is a chronic autoimmune disorder that results in patches of thick red skin with the appearance of silvery scales. These patches can be found on elbows, knees, scalp, low back, face, feet, fingernails, toenails and even the mouth. Psoriasis can be confused with other skin disease so a dermatologist is the best physician to diagnosis psoriasis. Treatments may include creams, ointments, ultraviolet light therapy and medication (Center for Disease Control and Prevention, 2018). To learn more, visit the Center for Disease Control and Prevention’s web page on psoriasis.
Injuries
Skin injuries set off a healing process that occurs in several overlapping stages.
- The first step to repairing damaged skin is the formation of a blood clot that helps stop the flow of blood and scabs over with time. Many different types of cells are involved in wound repair, especially if the surface area that needs repair is extensive.
- Before the basal stem cells of the stratum basale can recreate the epidermis, fibroblasts mobilize and divide rapidly to repair the damaged tissue by collagen deposition, forming granulation tissue.
- Blood capillaries follow the fibroblasts and help increase blood circulation and oxygen supply to the area.
- Immune cells, such as macrophages, roam the area and engulf any foreign matter to reduce the chance of infection (Betts, et al., 2021).
Burns
A burn results when the skin is damaged by intense heat, radiation, electricity, or chemicals. The damage results in the death of skin cells, which can lead to a massive loss of fluid. Dehydration, electrolyte imbalance, and renal and circulatory failure follow, which can be fatal. Burn patients are treated with intravenous fluids to offset dehydration, as well as intravenous nutrients that enable the body to repair tissues and replace lost proteins. Another serious threat to the lives of burn patients is infection. Burned skin is extremely susceptible to bacteria and other pathogens, due to the loss of protection by intact layers of skin (Betts, et al., 2021).
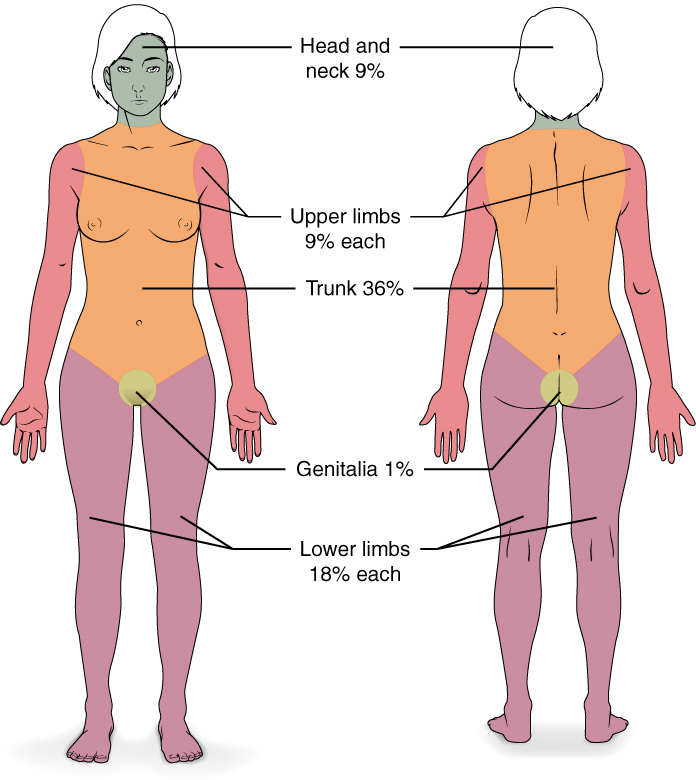
Burn Classification
Burns are sometimes measured in terms of the size of the total surface area affected. This is referred to as the rule of nines, which associates specific anatomical areas with a percentage that is a factor of nine (see Figure 3.16) (Betts, et al., 2021).
Burns are also classified by the degree of their severity.
- A first-degree burn is a superficial burn that affects only the epidermis. Although the skin may be painful and swollen, these burns typically heal on their own within a few days. Mild sunburn fits into the category of a first-degree burn.
- A second-degree burn goes deeper and affects both the epidermis and a portion of the dermis. These burns result in swelling and a painful blistering of the skin. It is important to keep the burn site clean and sterile to prevent infection. If this is done, the burn will heal within several weeks.
- A third-degree burn fully extends into the epidermis and dermis, destroying the tissue and affecting the nerve endings and sensory function. These are serious burns that may appear white, red, or black; they require medical attention and will heal slowly without it.
- A fourth-degree burn is even more severe, affecting the underlying muscle and bone.
Oddly, third and fourth-degree burns are usually not as painful because the nerve endings themselves are damaged. Full-thickness burns cannot be repaired by the body, because the local tissues used for repair are damaged and require debridement, or amputation in severe cases, followed by grafting of the skin from an unaffected part of the body, or from skin grown in tissue culture for grafting purposes. Skin grafts are required when the damage from trauma or infection cannot be closed with sutures or staples (Betts et al., 2021).
Scars and Keloids
Most cuts or wounds, with the exception of ones that only scratch the epidermis, lead to scar formation. Scarring occurs in cases in which there is repair of skin damage, but the skin fails to regenerate the original skin structure. Fibroblasts generate scar tissue in the form of collagen, and the bulk of repair is due to the basket-weave pattern generated by collagen fibers and does not result in regeneration of the typical cellular structure of skin. Instead, the tissue is fibrous in nature and does not allow for the regeneration of accessory structures, such as hair follicles, sweat glands, or sebaceous glands (Betts, et al., 2021).
Sometimes, there is an overproduction of scar tissue, because the process of collagen formation does not stop when the wound is healed; this results in a keloid (see Figure 3.17). In contrast, scars that result from acne and chickenpox have a sunken appearance and are called atrophic scars (Betts, et al., 2021).

Scarring of skin after wound healing is a natural process and does not need to be treated further. Application of mineral oil and lotions may reduce the formation of scar tissue. However, modern cosmetic procedures, such as dermabrasion, laser treatments, and filler injections have been invented as remedies for severe scarring. All of these procedures try to reorganize the structure of the epidermis and underlying collagen tissue to make it look more natural (Betts, et al., 2021).
Bedsores and Stretch Marks
Skin and its underlying tissue can be affected by excessive pressure. One example of this is called a bedsore. Bedsores, also called decubitis ulcers, are caused by constant, long-term, unrelieved pressure on certain body parts that are bony, reducing blood flow to the area and leading to necrosis . Bedsores are most common in elderly patients who have debilitating conditions that cause them to be immobile. Most hospitals and long-term care facilities have the practice of turning the patients every few hours to prevent the incidence of bedsores. If left untreated bedsores can be fatal if they become infected (Betts, et al., 2021)
The skin can also be affected by pressure associated with rapid growth. A stretch mark results when the dermis is stretched beyond its limits of elasticity, as the skin stretches to accommodate the excess pressure. Stretch marks usually accompany rapid weight gain during puberty and pregnancy. They initially have a reddish hue, but lighten over time. Other than for cosmetic reasons, treatment of stretch marks is not required. They occur most commonly over the hips and abdomen (Betts, et al., 2021). For detailed images of types of bedsores, see Minnesota Hospital Association’s Pressure Ulcer Staging Cards.
Calluses
When you wear shoes that do not fit well and are a constant source of abrasion on your toes, you tend to form a callus at the point of contact. This occurs because the basal stem cells in the stratum basale are triggered to divide more often to increase the thickness of the skin at the point of abrasion to protect the rest of the body from further damage. This is an example of a minor or local injury, and the skin manages to react and treat the problem independent of the rest of the body. Calluses can also form on your fingers if they are subject to constant mechanical stress, such as long periods of writing, playing string instruments, or video games. A corn is a specialized form of callus. Corns form from abrasions on the skin that result from an elliptical-type motion (Betts, et al., 2021).
Medical Terms in Context
Medical Specialties and Procedures Related to the Integumentary System
A dermatologist is a medical doctor with specialized training in treating diseases, disorders and injuries related to the integumentary system and its accessory structures. There are many dermatologic subspecialties such as cosmetic dermatology, dermatopathology and pediatric dermatology. To learn more visit the ‘What is a Dermatologist?’ page of the American Academy of Dermatology Association website.
Dermatologists can be specially trained to perform a procedure called Mohs surgery. Mohs surgery excises skin cancers in thin layers until all cancer is removed from the tissue (Mayo Clinic Staff, 2017). For more details about each step of the process visit the Skin Cancer Foundation’s site on Mohs Surgery.
Test Yourself
References
Centers for Disease Control and Prevention. (2018, October 25). Psoriasis. Centers for Disease Control and Prevention: Fungal Diseases. https://www.cdc.gov/psoriasis/
Centers for Disease Control and Prevention. (2018a, August 6). Ringworm. Centers for Disease Control and Prevention: Fungal Diseases. https://www.cdc.gov/fungal/diseases/ringworm/definition.html
CrashCourse. (2015, February 16). The Integumentary system, part 2 – skin deeper: Crash Course A&P #7 [Video]. YouTube. https://youtu.be/EN-x-zXXVwQ
Mayo Clinic Staff. (2017, September 6). Mohs surgery. Mayo Clinic. https://www.mayoclinic.org/tests-procedures/mohs-surgery/about/pac-20385222#:~:text=Mohs%20surgery%20is%20a%20precise,known%20as%20Mohs%20micrographic%20surgery.
Ted-Ed. (2018). The science of skin- Emma Bryce [Video]. https://www.youtube.com/watch?v=OxPlCkTKhzY&t=1s
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.
has numerous blood vessels
unconsciously regulates
flight or fight response
outer layer of skin, made of closely packed epithelial cells
The layer that is made of dense, irregular connective tissue that houses blood vessels, hair follicles, sweat glands, and other structures
Literally means below the dermis. The layer of the skin below the dermis that is composed mainly of loose connective and fatty tissues
without blood vessels
The number of times the heart contracts in one minute.
fat cells
Cells that engulf and absorb bacteria and cell particles
Tactile corpsucle that responds to light and touch, touch receptors.
net like
fibrous tissue
WTCS Learning Objectives
- Apply the rules of medical language to build, analyze, spell, pronounce, abbreviate, and define terms as they relate to the lymph and immune systems
- Identify meanings of key word components of the lymph and immune systems
- Categorize diagnostic, therapeutic, procedural or anatomic terms related to the lymph and immune systems
- Use terms related to the lymph and immune systems
- Use terms related to the diseases and disorders of the lymph and immune systems
Word Parts for the Lymphatic and Immune Systems
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Lymphatic and Immune Systems.
Introduction to the Lymphatic and Immune Systems
The lymphatic system is a series of vessels, ducts, and trunks that remove interstitial fluid from the tissues and return it the blood. The lymphatic vessels are also used to transport dietary lipids and cells of the immune system. Cells of the immune system, lymphocytes, all come from the hematopoietic system of the bone marrow. Primary lymphoid organs, the bone marrow and thymus gland, are the locations where lymphocytes proliferate and mature. Secondary lymphoid organs are the site in which mature lymphocytes congregate to mount immune responses. Many immune system cells use the lymphatic and circulatory systems for transport throughout the body to search for and then protect against pathogens.
This chapter begins by describing the anatomy and physiology of the lymphatic system, whose immune functions lead us into a discussion of the body's multifaceted defenses, which together make up the immune system. Since the lymphatic system shares organs with a number of other body systems, the pathology discussed near the end of this chapter mainly focuses on disorders of the immune system.
Watch this video:
Media 11.1 Lymphatic System: Crash Course A&P #44 [Online video]. Copyright 2015 by CrashCourse.
Lymphatic and Immune Systems Medical Terms
Anatomy and Physiology of the Lymphatic System
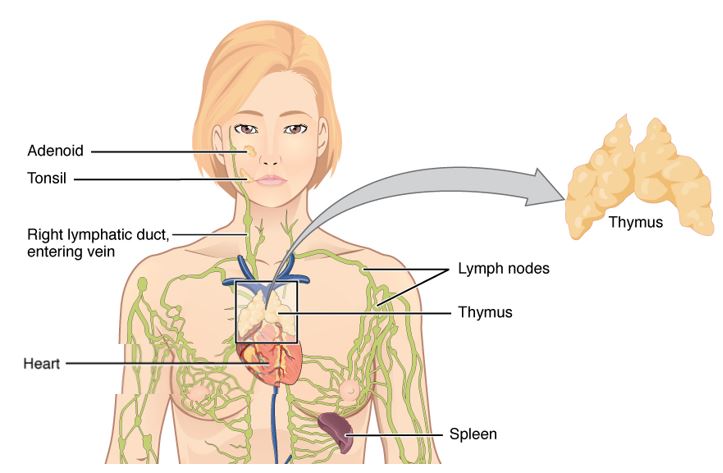
The lymphatic vessels begin as open-ended capillaries, which feed into larger and larger lymphatic vessels, and eventually empty into the bloodstream. Along the way, the lymph travels through the lymph nodes, which are commonly found near the groin, armpits, neck, chest, and abdomen. Humans have about 500–600 lymph nodes throughout the body (see Figure 11.1). Several organs and tissues that participate in immunity are also part of the lymphatic system.
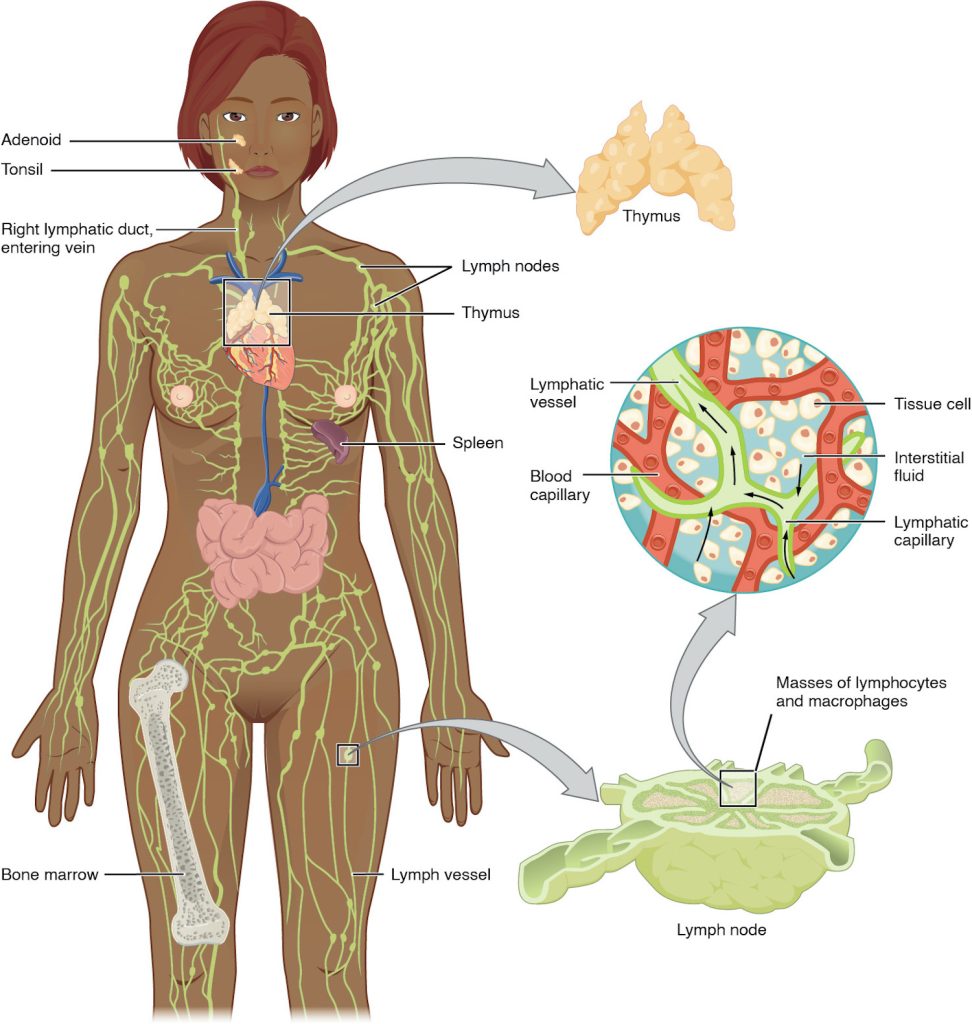
Lymphatic Capillaries
An important function of the lymphatic system is to return the fluid (lymph) to the blood. Lymph may be thought of as recycled blood plasma. Blood pressure causes leakage of fluid from the blood capillaries, resulting in the accumulation of fluid in the interstitial space. In humans, 20 liters of plasma is released into the interstitial space of the tissues each day due to capillary leakage. The blood vessels reabsorb 17 liters of this interstitial fluid, leaving three liters in the tissues for the lymphatic system to transport back to the circulation. If the lymphatic system is damaged in some way, such as by being blocked by cancer cells or destroyed by injury, interstitial fluid accumulates in the tissue spaces, causing a condition called lymphedema.
Lymphatic capillaries, also called the terminal lymphatics, are vessels where interstitial fluid enters the lymphatic system to become lymph. Located in almost every tissue in the body, these vessels are interlaced among the arterioles and venules of the circulatory system in the soft connective tissues of the body. See Figure 11.2. Exceptions are the central nervous system, bone marrow, bones, teeth, and the cornea of the eye, which do not contain lymph vessels.
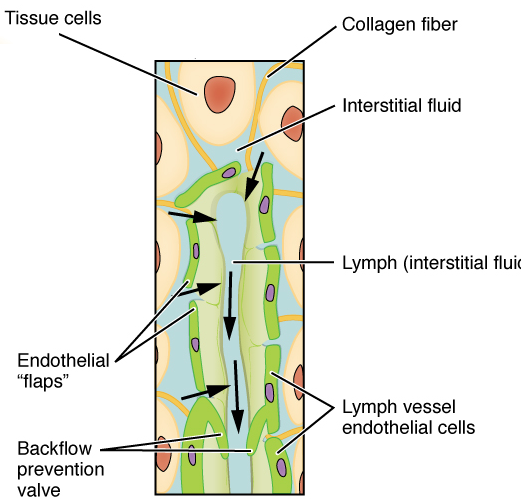
Larger Lymphatic Vessels, Trunks, and Ducts
The lymphatic capillaries empty into larger lymphatic vessels, which are similar to veins in terms of their three-tunic structure and the presence of valves. These one-way valves are located fairly close to one another, and each one causes a bulge in the lymphatic vessel, giving the vessels a beaded appearance (see Figure 11.2).
In general, superficial lymphatics, follow the same routes as veins, whereas deep lymphatic vessels of the viscera generally follow the paths of arteries. The superficial and deep lymphatics eventually merge to form larger lymphatic structures known as lymphatic trunks. On the right side of the body, the right sides of the head, thorax, and right upper limb trunks drain lymph fluid into the right subclavian vein via the right lymphatic duct (see Figure 11.3). On the left side of the body, the trunks from the remaining portions of the body drain into the larger thoracic duct, which drains into the left subclavian vein. The thoracic duct itself begins just beneath the diaphragm in the cisterna chyli.
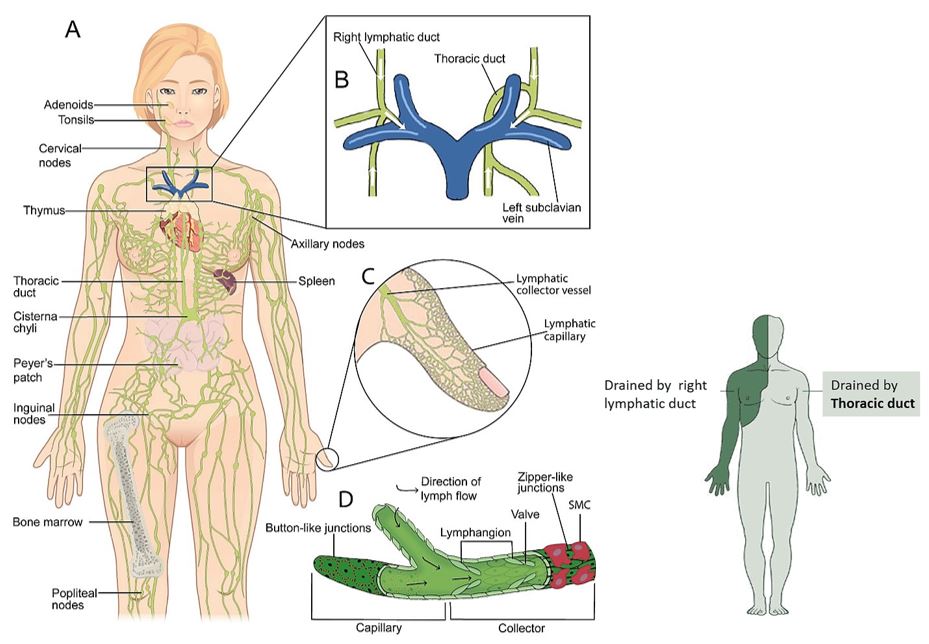
Primary Lymphoid Organs
The primary lymphoid organs are the bone marrow and thymus gland. The lymphoid organs are where lymphocytes mature, proliferate, and are selected, which enables them to attack pathogens without harming the cells of the body.
- Bone Marrow
- Recall that all blood cells, including lymphocytes, are formed in the red bone marrow. The B cell undergoes nearly all of its development in the red bone marrow, whereas the immature T cell, called a thymocyte, leaves the bone marrow and matures largely in the thymus gland.
- Thymus
- The thymus gland, where T cells mature, is a bilobed organ found in the space between the sternum and the aorta of the heart (see Figure 11.4). Connective tissue holds the lobes closely together but also separates them and forms a capsule.
- The loss of immune function with age is called immunosenescence. One major cause of age-related immune deficiencies is thymic involution.
- The shrinking of the thymus gland begins at birth at a rate of about three percent tissue loss per year. This shrinking continues until 35–45 years of age then the rate declines to about one percent loss per year for the rest of one’s life. At that pace, the total loss of thymic epithelial tissue and thymocytes would occur at about 120 years of age. So, in theory, 120 years could be the maximum life span.
Concept Check
- Do you remember what the suffix "-oid" means?
- Can you explain the term lymphoid?
Secondary Lymphoid Organs
Lymphocytes develop and mature in the primary lymphoid organs, but they mount immune responses from the secondary lymphoid organs, which include the lymph nodes, spleen, and lymphoid nodules. A naïve lymphocyte is one that has left the primary organ, where it learned to function immunologically, and entered a secondary lymphoid organ where it waits to encounter an antigen against which it will mount a response.
Lymph Nodes
Lymph nodes function to remove debris and pathogens from the lymph, and are thus sometimes referred to as the “filters of the lymph” (see Figure 11.6). Any bacteria that infect the interstitial fluid are taken up by the lymphatic capillaries and transported to a regional lymph node. Dendritic cells and macrophages within this organ internalize and kill many of the pathogens that pass through, thereby removing them from the body. The lymph node is also the site of adaptive immune responses mediated by T cells, B cells, and accessory cells of the adaptive immune system.
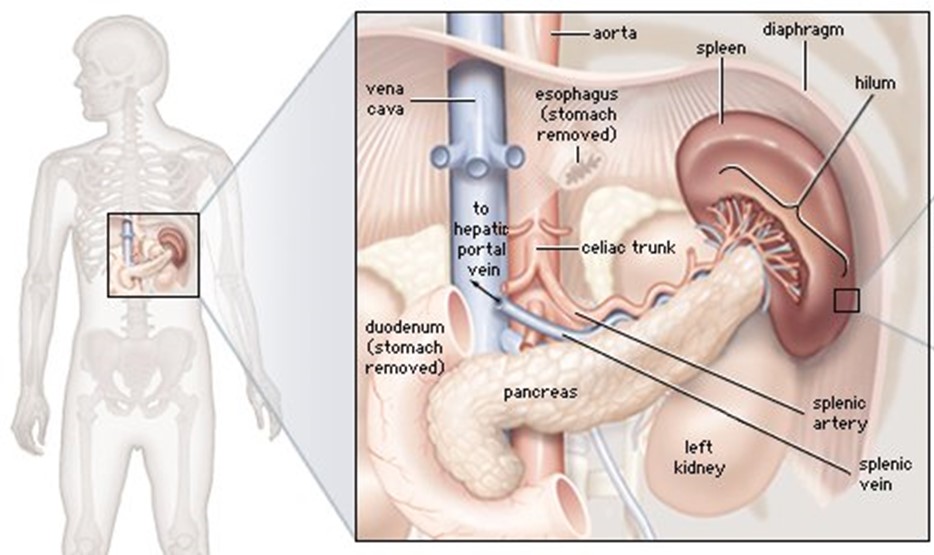
Spleen
The spleen is a vascular organ that is somewhat fragile due to the absence of a capsule. It is about 12 cm long and is attached to the lateral border of the stomach. The spleen is sometimes called the “filter of the blood” because of its extensive vascularization and the presence of macrophages and dendritic cells that remove microbes and other materials from the blood, including dying red blood cells. The spleen also functions as the location of immune responses to blood-borne pathogens. (See Fig 11.6).
Lymphoid Nodules
The other lymphoid tissues, the lymphoid nodules, consist of a dense cluster of lymphocytes without a surrounding fibrous capsule. These nodules are located in the respiratory and digestive tracts, areas routinely exposed to environmental pathogens.
Tonsils are lymphoid nodules located along the inner surface of the pharynx and are important in developing immunity to oral pathogens (see Figure 11.7). The tonsil located at the back of the throat, the pharyngeal tonsil, is sometimes referred to as the adenoid when swollen. Such swelling is an indication of an active immune response to infection. Tonsils have deep grooves called crypts, which accumulate all sorts of materials taken into the body through eating and breathing and actually “encourage” pathogens to penetrate deep into the tonsillar tissues where they are eliminated. A major function of tonsils is to help children’s bodies recognize, destroy, and develop immunity to common environmental pathogens so that they will be protected in their later lives. Tonsils are often removed in children who have recurring throat infections since swollen palatine tonsils can interfere with breathing and/or swallowing.
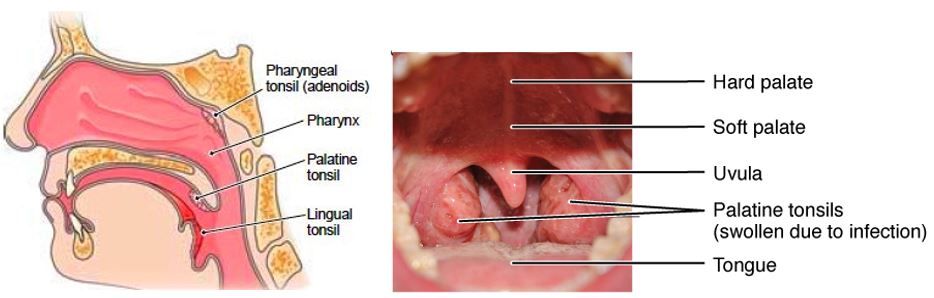
Concept Check
Tonsils are named after their locations.
- Look at the figure above and determine which anatomical structure is closely associated with each set of tonsils and was therefore used to name the tonsils, for example, the lingual tonsils are named after the tongue (lingula).
- Can you tell which structures were used to name the palatine tonsils and the pharyngeal tonsils?
Watch this video:
Media 11.2 Immune System, Part 1: Crash Course A&P #45 [Online video]. Copyright 2015 by CrashCourse.
Cells of the Innate Immune Response
Phagocytes: Macrophages and Neutrophils
A phagocyte is a cell that is able to surround and engulf a particle or cell, a process called phagocytosis. The phagocytes of the immune system engulf other particles or cells, either to clean an area of debris, old cells, or to kill pathogenic organisms such as bacteria. Macrophages, neutrophils, and dendritic cells are the major phagocytes of the immune system and are the body’s fast acting, front line immunological defense against organisms that have breached barrier defenses and have entered the body.
Macrophages not only participate in innate immune responses but have also evolved to cooperate with lymphocytes as part of the adaptive immune response. Macrophages exist in many tissues of the body, either freely roaming through connective tissues or fixed to reticular fibers within specific tissues such as lymph nodes. When pathogens breach the body’s barrier defenses, macrophages are the first line of defense.
A neutrophil is a phagocytic cell that is attracted via chemotaxis from the bloodstream to infected tissues. contains cytoplasmic granules, which in turn contain a variety of vasoactive mediators such as histamine. Whereas macrophages act like sentries, always on guard against infection, neutrophils can be thought of as military reinforcements that are called into a battle to hasten the destruction of the enemy.
A monocyte is a circulating precursor cell that differentiates into either a macrophage or dendritic cell, which can be rapidly attracted to areas of infection by signal molecules of inflammation.
Natural Killer Cells
NK cells are a type of lymphocyte that have the ability to induce apoptosis in cells infected with pathogens such as intracellular bacteria and viruses. If apoptosis is induced before the virus has the ability to synthesize and assemble all its components, no infectious virus will be released from the cell, thus preventing further infection.
Concept Check
Do you know the difference between these terms?
Cytokines and Chemokines
A cytokine is signaling molecule that allows cells to communicate with each other over short distances. Cytokines are secreted into the intercellular space, and the action of the cytokine induces the receiving cell to change its physiology. A chemokine is a soluble chemical mediator similar to cytokines except that its function is to attract cells (chemotaxis) from longer distances.
Early Induced Proteins
Early induced proteins are those that are not constitutively present in the body, but are made as they are needed early during the innate immune response. Interferons are an example of early induced proteins. Cells infected with viruses secrete interferons that travel to adjacent cells and induce them to make antiviral proteins. Thus, even though the initial cell is sacrificed, the surrounding cells are protected.
Inflammatory Response
The hallmark of the innate immune response is inflammation. Stub a toe, cut a finger, or do any activity that causes tissue damage and inflammation will result, with its four characteristics: heat, redness, pain, and swelling (“loss of function” is sometimes mentioned as a fifth characteristic). It is important to note that inflammation does not have to be initiated by an infection, but can also be caused by tissue injuries. The release of damaged cellular contents into the site of injury is enough to stimulate the response, even in the absence of breaks in physical barriers that would allow pathogens to enter (by hitting your thumb with a hammer, for example). The inflammatory reaction brings in phagocytic cells to the damaged area to clear cellular debris and encourages the entry of clotting factors to set the stage for wound repair. Inflammation also facilitates the transport of antigen to lymph nodes by dendritic cells for the development of the adaptive immune response. (Fig. 11.8).
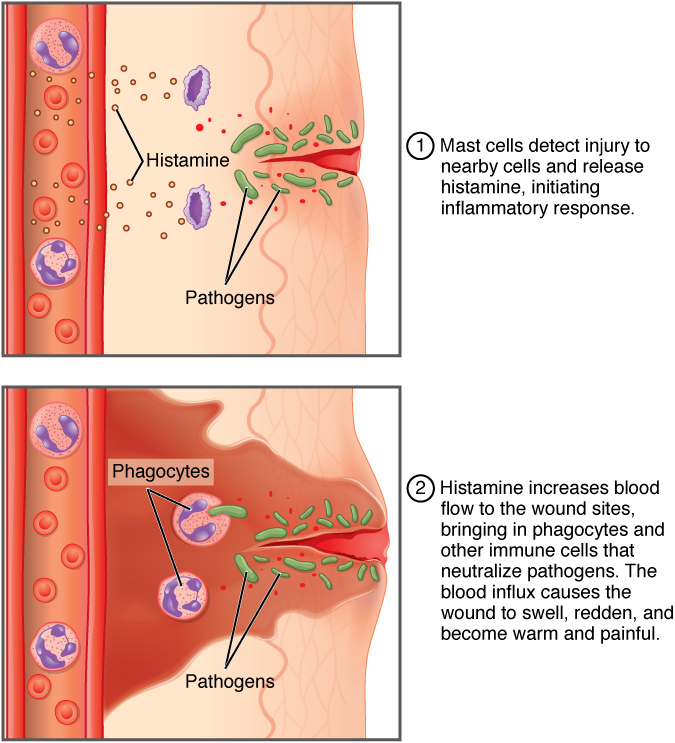
The above image summarizes the following events in the inflammatory response:
-
- The released contents of injured cells stimulate the release of substances from mast cells including histamine, leukotrienes, and prostaglandins.
-
- Histamine increases blood flow to the area by vasodilation, resulting in heat and redness. Histamine also increases the permeability of local capillaries, causing plasma to leak out and form interstitial fluid, resulting in swelling
-
- Leukotrienes attract neutrophils from the blood by chemotaxis.
When local infections are severe, neutrophils are attracted to the sites of infections in large numbers, and as they phagocytose the pathogens and subsequently die, their accumulated cellular remains are visible as pus at the infection site.
- Leukotrienes attract neutrophils from the blood by chemotaxis.
-
- Prostaglandins cause vasodilation by relaxing vascular smooth muscle and are a major cause of the pain associated with inflammation. Nonsteroidal anti-inflammatory drugs such as aspirin and ibuprofen relieve pain by inhibiting prostaglandin production.
Concept Check
- Do you remember the suffix used to describe 'inflammation'?
- Describe what causes the pain associated with inflammation.
Acute inflammation is a short-term innate immune response to an insult to the body. If the cause of the inflammation is not resolved, however, it can lead to chronic inflammation, which is associated with major tissue destruction and fibrosis.
Phase 3: Adaptive Immune Response
Watch this video:
Media 11.3 Immune System, Part 2: Crash Course A&P #46 [Online video]. Copyright 2015 by CrashCourse.
Benefits of the Adaptive Immune Response
- Specificity
- The ability to specifically recognize and mount a response against almost any pathogen.
- Antigens, are recognized by receptors on the surface of B and T lymphocytes.
- Immunological Memory
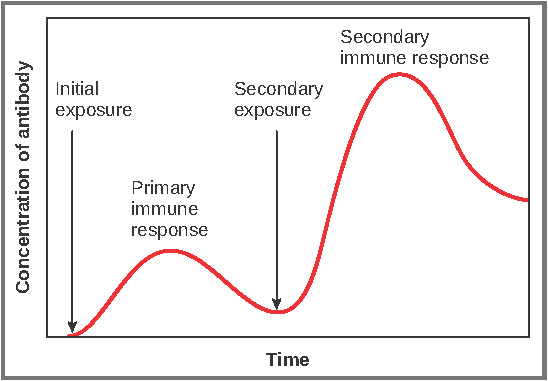
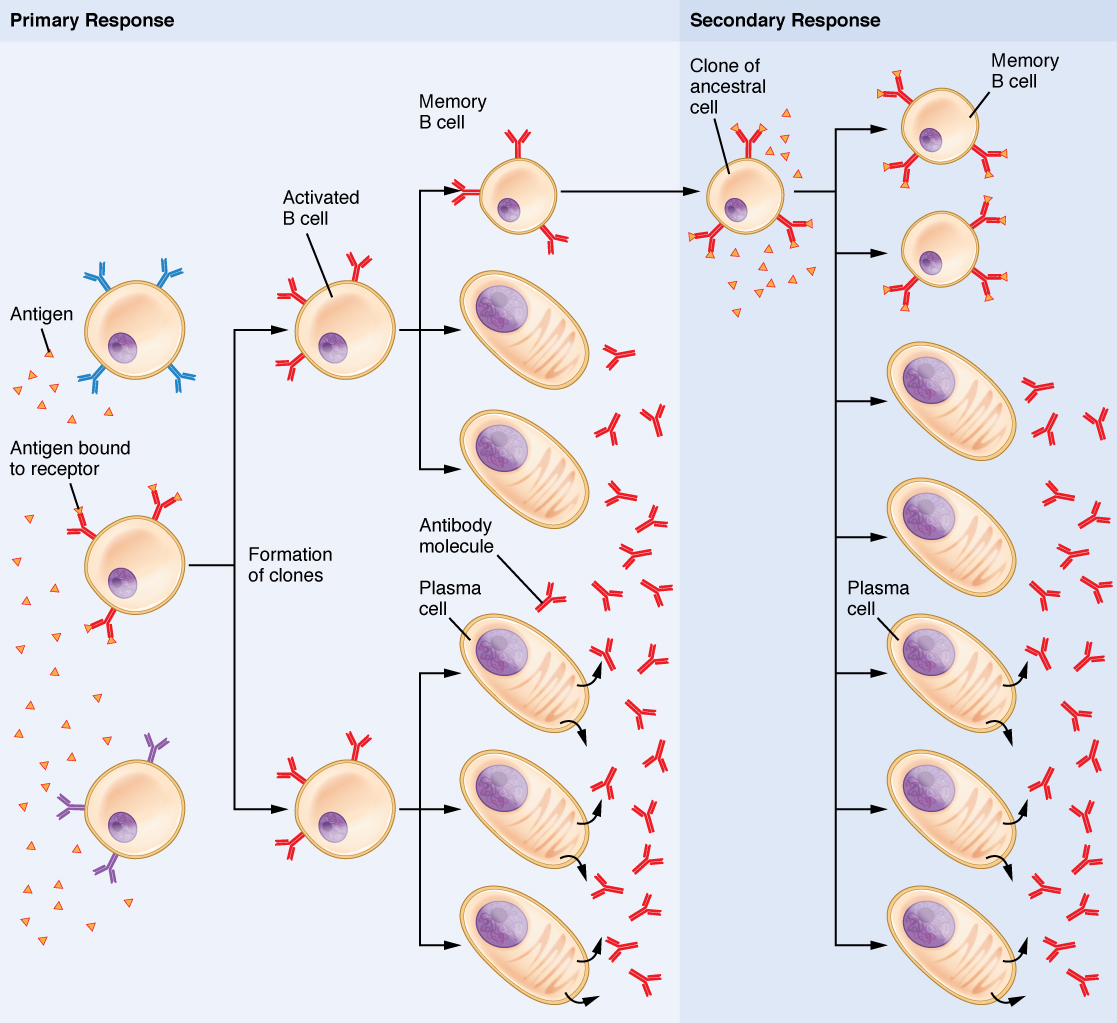
- The first exposure to a pathogen is called a primary adaptive response.
- Symptoms of a first infection, called primary disease, are always relatively severe because it takes time for an initial adaptive immune response to a pathogen to become effective.
- Upon re-exposure to the same pathogen, a secondary adaptive immune response is generated, which is stronger and faster that the primary response, often eliminating the pathogen before it can cause damage or even symptoms.
- This secondary response is the basis of immunological memory, which gives us immunity.
- Self Recognition
- The ability to distinguish between self-antigens, those that are normally present in the body, and foreign antigens, those that might be on a potential pathogen.
- As T and B cells mature, there are mechanisms in place that prevent them from recognizing self-antigen, preventing a damaging immune response against the body. When these mechanisms fail, their breakdown leads to autoimmune diseases.
Lymphocytes: B Cells, T Cells, Plasma Cells
As stated above, lymphocytes are the primary cells of adaptive immune responses. These cells were introduced in the previous chapter and are summarized in the following table:
| CELL TYPE | DESCRIPTION AND DETAILS |
| Plasma Cell | B cell (lymphocyte) that has been activated through exposure to an antigen and produces antibodies against that antigen (see the figure below) There are 5 classes of antibodies (IgM, IgG, IgE, IgA, IgD), each functioning in different ways: IgM promotes chemotaxis, opsonization, and cell lysis, making it a very effective antibody against bacteria at early stages of a primary antibody response IgG is the one that crosses the placenta to protect the developing fetus from disease and exits the blood to the interstitial fluid to fight extracellular pathogens IgA is the only antibody to leave the interior of the body to protect body surfaces. IgA is also of importance to newborns, because this antibody is present in mother’s breast milk (colostrum), which serves to protect the infant IgE is associated with allergies and anaphylaxis |
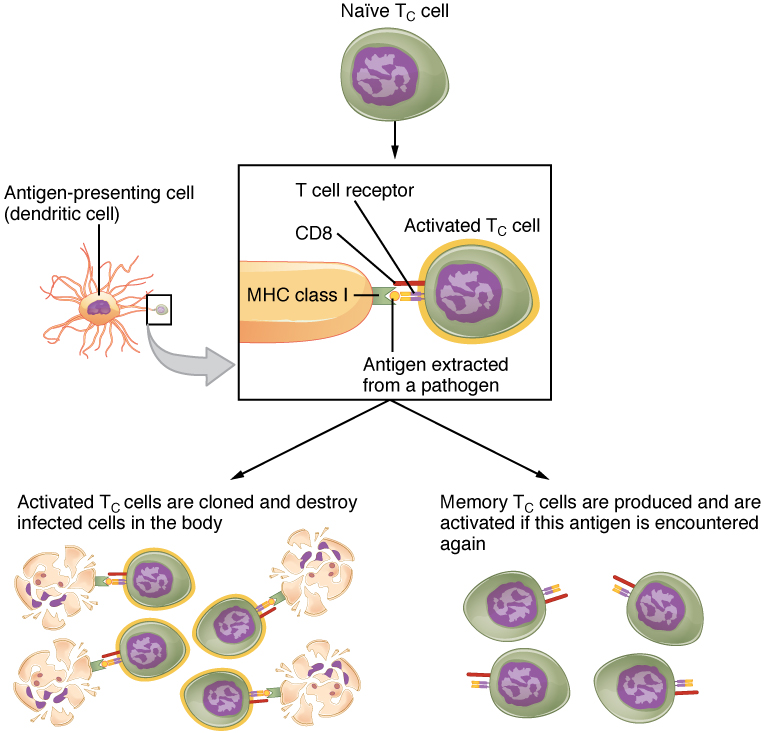
| T Cell | Different T cell types have the ability to either secrete soluble factors that communicate with other cells of the adaptive immune response or destroy cells infected with intracellular pathogen
|
| Memory Cell | B cells and T cells formed during primary exposure to a pathogen (see the figure below) Remain in the body for a long time after an infection and are able to mount a fast and effective immune response to a pathogen if it is encountered a second time, preventing the pathogen from causing disease |
Active Versus Passive Immunity
Immunity to pathogens, and the ability to control pathogen growth so that damage to the tissues of the body is limited, can be acquired by:
- The active development of an immune response in the infected individual.
or - The passive transfer of immune components from an immune individual to a non-immune one.
The downside to this passive immunity is the lack of the development of immunological memory. Once the antibodies are transferred, they are effective for only a limited time before they degrade.
| IMMUNITY | NATURAL | ARTIFICIAL |
|---|---|---|
| Active: resistance to pathogens acquired during an adaptive immune response | Result of memory cells formed during the adaptive immune response to a pathogen | Vaccine response. Through vaccination, one avoids the disease that results from the first exposure to the pathogen, yet reaps the benefits of protection from immunological memory. Vaccination was one of the major medical advances of the twentieth century and led to the eradication of smallpox and the control of many infectious diseases, including polio, measles, and whooping cough |
| Passive: transfer of antibodies from an immune person to a nonimmune person | Trans-placental antibodies from mother to fetus and maternal antibodies in breast milk protect newborn from infections | Immunoglobulin injections taken from animals previously exposed to a specific pathogen; a fast-acting method of temporarily protecting an individual who was possibly exposed to a pathogen |
Evasion of the Immune System by Pathogens
The immune system and pathogens are in a slow, evolutionary race to see who stays on top. Early childhood is a time when the body develops much of its immunological memory that protects it from diseases in adulthood. Pathogens have shown the ability, however, to evade the body’s immune responses, as described below.
-
- Protective adaptations: It is important to keep in mind that although the immune system has evolved to be able to control many pathogens, pathogens themselves have evolved ways to evade the immune response. An example is in Mycobactrium tuberculosis, which has evolved a complex cell wall that is resistant to the digestive enzymes of the macrophages that ingest them, and thus persists in the host, causing the chronic disease tuberculosis.
-
- Multiple strains: Bacteria sometimes evade immune responses because they exist in multiple strains, each having different surface antigens and requiring individual adaptive immune responses. One example is a small group of strains of S. aureus, called methicillin-resistant Staphylococcus aureus (MRSA), which has become resistant to multiple antibiotics..
-
- Antigen mutation: Because viruses’ surface molecules mutate continuously, viruses like influenza change enough each year that the flu vaccine for one year may not protect against the flu common to the next. New vaccine formulations must be derived for each flu season.
-
- Genetic recombination: An example is the influenza virus, which contains gene segments that can recombine when two different viruses infect the same cell. Recombination between human and pig influenza viruses led to the 2010 H1N1 swine flu outbreak.
-
- Immunosuppression: Pathogens, especially viruses, can produce immunosuppressive molecules that impair immune function.
Tissue Transplantation
Immunosuppressive drugs such as cyclosporine A have made transplants more successful, but tissue matching is still key. Family members, since they share a similar genetic background, are much more likely to share MHC molecules than unrelated individuals do.
One disease of transplantation occurs with bone marrow transplants, which are used to treat various diseases, including SCID and leukemia. Because the bone marrow cells being transplanted contain lymphocytes capable of mounting an immune response, and because the recipient’s immune response has been destroyed before receiving the transplant, the donor cells may attack the recipient tissues, causing graft-versus-host disease. Symptoms of this disease, which usually include a rash and damage to the liver and mucosa, are variable, and attempts have been made to moderate the disease by first removing mature T cells from the donor bone marrow before transplanting it.
Immune Responses Against Cancer
It is clear that with some cancers, like Kaposi’s sarcoma (see Figure 11.11), for example, that a healthy immune system does a good job at controlling them. This disease, which is caused by the human herpes virus, is almost never observed in individuals with strong immune systems. Other examples of cancers caused by viruses include liver cancer caused by the hepatitis B virus and cervical cancer caused by the human papilloma virus. As these last two viruses have vaccines available for them, getting vaccinated can help prevent these two types of cancer by stimulating the immune response.

On the other hand, as cancer cells are often able to divide and mutate rapidly, they may escape the immune response, just as certain pathogens such as HIV do.
There are three stages in the immune response to many cancers:
-
- Elimination occurs when the immune response first develops toward tumor-specific antigens specific to the cancer and actively kills most cancer cells.
- Equilibrium is the period that follows, during which the remaining cancer cells are held in check.
- Escape of the immune response, and resulting disease, occurs because many cancers mutate and no longer express any specific antigens for the immune system to respond to.
This fact has led to extensive research in trying to develop ways to enhance the early immune response to completely eliminate the early cancer and thus prevent a later escape. One method that has shown some success is the use of cancer vaccines. These differ from other vaccines in that they are directed against the cells of one’s own body. Treated cancer cells are injected into cancer patients to enhance their anti-cancer immune response and thereby prolong survival. The immune system has the capability to detect these cancer cells and proliferate faster than the cancer cells do, thus overwhelming the cancer in a similar way as they do for viruses. Cancer vaccines are being developed for malignant melanoma and renal (kidney) cell carcinoma.
Immune Responses and Stress
In order to protect the entire body from infection, the immune system is required to interact with other organ systems, sometimes in complex ways. For example, hormones such as cortisol (naturally produced by the adrenal cortex) and prednisone (synthetic) are well known for their abilities to suppress T cell immune mechanisms, hence, their prominent use in medicine as long-term, anti-inflammatory drugs.
One well-established interaction of the immune, nervous, and endocrine systems is the effect of stress on immune health. In the human vertebrate evolutionary past, stress was associated with the fight-or-flight response, largely mediated by the central nervous system and the adrenal medulla. This stress was necessary for survival since fighting or fleeing usually resolved the problem in one way or another. It has been found that short-term stress diverts the body’s resources towards enhancing innate immune responses. This has the ability to act fast and would seem to help the body prepare better for possible infections associated with the trauma that may result from a fight-or-flight exchange.
On the other hand, there are no physical actions to resolve most modern day stresses, including short-term stressors like taking examinations and long-term stressors such as being unemployed or losing a spouse. The effect of stress can be felt by nearly every organ system, and the immune system is no exception (see Table 11.3). Chronic stress, unlike short-term stress, may inhibit immune responses even in otherwise healthy adults. The suppression of both innate and adaptive immune responses is clearly associated with increases in some diseases.
| SYSTEM | STRESS-RELATED ILLNESS |
|---|---|
| Integumentary system | Acne, skin rashes, irritation |
| Nervous system | Headaches, depression, anxiety, irritability, loss of appetite, lack of motivation, reduced mental performance |
| Muscular and skeletal systems | Muscle and joint pain, neck and shoulder pain |
| Circulatory system | Increased heart rate, hypertension, increased probability of heart attacks |
| Digestive system | Indigestion, heartburn, stomach pain, nausea, diarrhea, constipation, weight gain or loss |
| Immune system | Depressed ability to fight infections |
| Male reproductive system | Lowered sperm production, impotence, reduced sexual desire |
| Female reproductive system | Irregular menstrual cycle, reduced sexual desire |
Anatomy Labeling Activity
Medical Terms not Easily Broken into Word Parts
Lymphatic and Immune System Abbreviations
Diseases and Disorders of the Lymphatic and Immune Systems
The immune response can be under-reactive or over-reactive, leading to a state of disease. The factors that maintain immunological homeostasis are complex and incompletely understood.
Underactive Immune System: Immunodeficiencies
Suppressed immunity can result from inherited genetic defects or by acquiring viruses (Betts, et al., 2021).
Inherited Immunodeficiencies/SCID
New treatments for SCID using gene therapy, inserting nondefective genes into cells taken from the patient and giving them back, have the advantage of not needing the tissue match required for standard transplants. Although not a standard treatment, this approach holds promise, especially for those in whom standard bone marrow transplantation has failed (Betts, et al., 2021).
Acquired Immunodeficiency/HIV and AIDS
After seroconversion, the amount of virus circulating in the blood drops and stays at a low level for several years. During this time, the levels of CD4 T cells decline steadily, until at some point, the immune response is so weak that opportunistic disease and eventually death result.
Treatment for the disease consists of drugs that target virally encoded proteins that are necessary for viral replication but are absent from normal human cells. By targeting the virus itself and sparing the cells, this approach has been successful in significantly prolonging the lives of HIV-positive individuals (Betts, et al., 2021).
Overactive Immune System: Hypersensitivities and Autoimmune Diseases
Hypersensitivities
| TYPE OF HYPERSENSITIVITY | DETAILS AND EXPLANATION |
| Type I |
|
| Type II |
|
| Type III |
|
| Type IV |
|
Autoimmune Responses
The worst cases of the immune system over-reacting are autoimmune diseases in which the immune systems begin to attack cells of the patient's own body, causing chronic inflammation and significant damage. The trigger for these diseases is often unknown, although environmental and genetic factors are likely involved. Treatments are usually based on resolving the symptoms using immunosuppressive and anti-inflammatory drugs. Figure 11.12 below provides two examples of autoimmune diseases: rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) (Betts, et al., 2021).
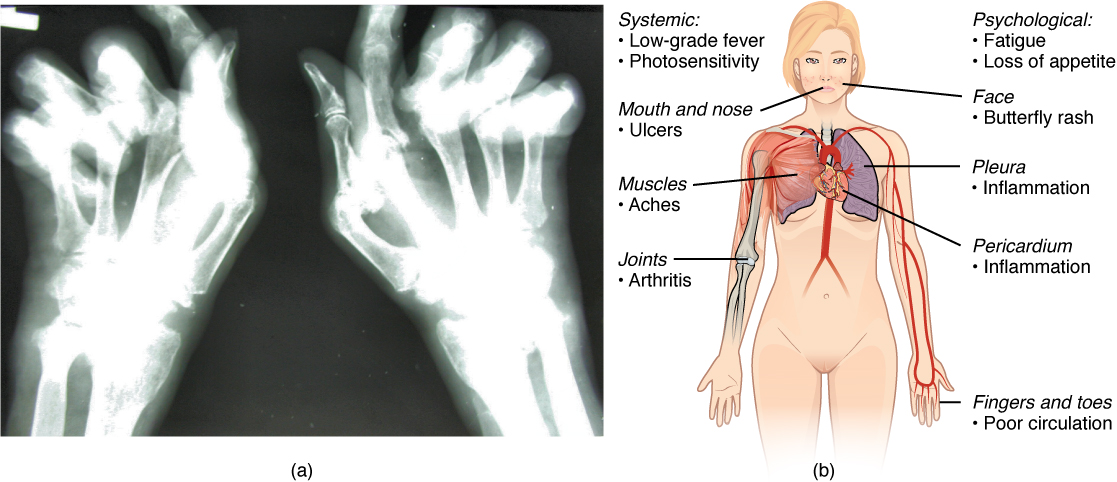
Overall, there are more than 80 different autoimmune diseases, which are a significant health problem in the elderly. Table 14.5 below lists several of the most common autoimmune diseases, the antigens that are targeted (autoantigen or "self" antigen), and the resulting tissue damage (Betts, et al., 2021).
| DISEASE | AUTOANTIGEN | SYMPTOMS |
|---|---|---|
| Celiac disease | Tissue transglutaminase | Damage to small intestine |
| Diabetes mellitus type I | Beta cells of pancreas | Low insulin production; inability to regulate serum glucose |
| Graves’ disease | Thyroid-stimulating hormone receptor (antibody blocks receptor) | Hyperthyroidism |
| Hashimoto’s thyroiditis | Thyroid-stimulating hormone receptor (antibody mimics hormone and stimulates receptor) | Hypothyroidism |
| Lupus erythematosus | Nuclear DNA and proteins | Damage of many body systems |
| Myasthenia gravis | Acetylcholine receptor in neuromuscular junctions | Debilitating muscle weakness |
| Rheumatoid arthritis | Joint capsule antigens | Chronic inflammation of joints |
Lymphoma
Lymphoma was briefly discussed in the previous chapter.
Medical Terms in Context
Medical Specialties and Procedures Related to the Lymphatic and Immune Systems
Clinical Immunology/Allergy is a medical specialty that diagnoses and treats diseases of the immune system (American Academy of Allergy Asthma and Immunology, 2021). For more information, please visit the 'About Careers in Allergy/Immunology' page from the American Academy of Allergy Asthma and Immunology.
Skin testing (for allergies) is done by a clinical immunologist/allergist to identify allergens in Type I hypersensitivity. In skin testing, allergen extracts are injected into the epidermis, and a positive result of the wheal and flare response usually occurs within 30 minutes. The soft center is due to fluid leaking from the blood vessels and the redness is caused by the increased blood flow to the area that results from the dilation of local blood vessels at the site (Betts, et al., 2021).
-
-
-
-
Test Yourself
References
American Academy of Allergy Asthma and Immunology. (2021). About Careers in Allergy/Immunology. https://www.aaaai.org/Professional-Education/careers-in-a-i
[CrashCourse]. (2015, November 30). Lymphatic system: Crash course A&P #44 [Video]. YouTube. https://youtu.be/I7orwMgTQ5I
[CrashCourse]. (2015, December 8). Immune system, part 1: Crash course A&P #45 [Video]. YouTube. https://youtu.be/GIJK3dwCWCw
[CrashCourse]. (2015, December 14). Immune system, part 2: Crash course A&P #46 [Video]. YouTube. https://youtu.be/2DFN4IBZ3rI
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.
-
-
-
tactile corpuscle that responds to light and touch, touch receptor
lamellated corpuscle that responds to vibration
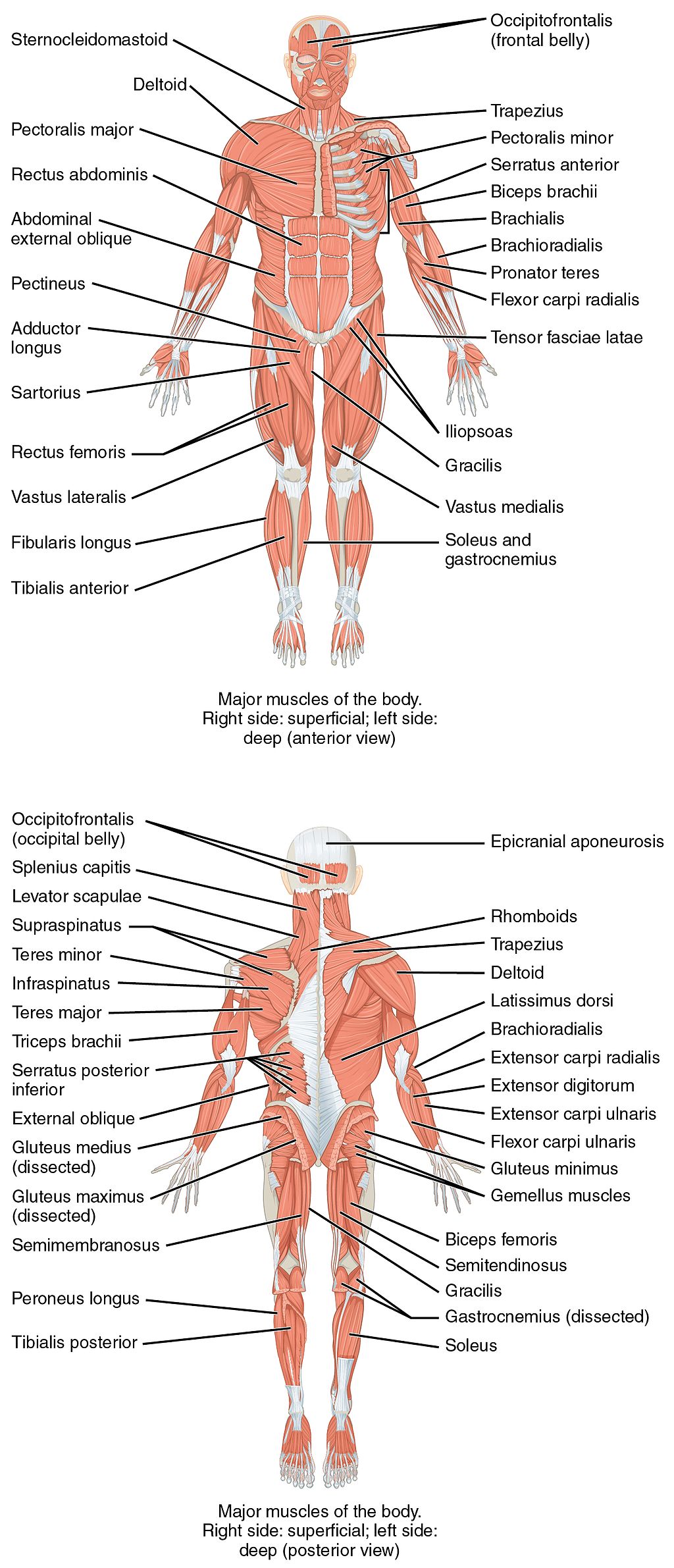
Learning Objectives
- Identify the anatomy of the muscular system
- Describe the main functions of the muscular system
- Spell the medical terms of the muscular system and use correct abbreviations
- Explore common diseases, disorders, and procedures related to the muscular system
- Identify the medical specialties associated with the muscular system
Muscular System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Muscular System.
Introduction to the Muscular System
When most people think of muscles, they think of the muscles that are visible just under the skin, particularly of the limbs. These are skeletal muscles, so-named because most of them move the skeleton. But there are two additional types of muscles: the smooth muscle and the cardiac muscle. The body has over 600 muscles which contribute significantly to the body's weight.
Watch this video:
Media 14.1 Muscles, Part 2 - Organismal Level: Crash Course A&P #22 [Online video]. Copyright 2015 by CrashCourse.
Muscular System Medical Terms
Anatomy (Structures) of the Muscular System
Muscle is one of the four primary tissue types of the body, and it is made up of specialized cells called fibers. The body contains three types of muscle tissue: skeletal muscle, , cardiac muscle, and smooth muscle (see Figure 14.1). All three muscle tissues have some properties in common; they all exhibit a quality called excitability as their plasma membranes can change their electrical states (from polarized to depolarized) and send an electrical wave called an action potential along the entire length of the membrane. Fascia is fibrous connective tissue that encloses muscles.
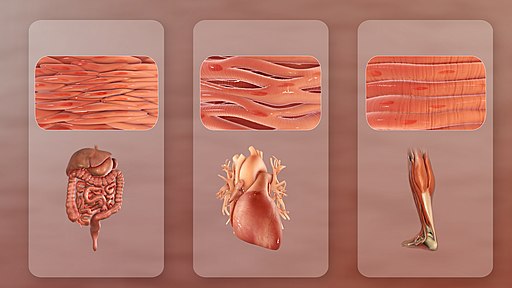
Three Types of Muscle Tissues
- Smooth - mainly associated with the walls of the internal organs. Also known as visceral muscles and are responsible for involuntary muscle movement - such as breathing, etc.
- Cardiac - heart muscle or myocardium. Its appearance is similar to a skeletal muscle and is responsible for the pumping of blood. It gives the heart beat.
- Skeletal - closely associated with the skeletal system. Also known as striated muscles and are responsible for voluntary muscle movement - such as swallowing, etc.
Smooth Muscle
Smooth muscle, so named because the cells do not have striations, is present in the walls of hollow organs like the urinary bladder, uterus, stomach, intestines, and in the walls of passageways, such as the arteries and veins of the circulatory system, and the tracts of the respiratory, urinary, and reproductive systems. Smooth muscle is also present in the eyes, where it functions to change the size of the iris and alter the shape of the lens; and in the skin where it causes hair to stand erect in response to cold temperature or fear.
Cardiac Muscle
Cardiac muscle tissue is only found in the heart. Highly coordinated contractions of cardiac muscle pump blood into the vessels of the circulatory system. Similar to skeletal muscle, cardiac muscle is striated and organized into sarcomeres, possessing the same banding organization as skeletal muscle (see Figure 14.1). Cardiac muscle fibers cells also are extensively branched and are connected to one another at their ends by intercalated discs. An intercalated disc allows the cardiac muscle cells to contract in a wave-like pattern so that the heart can work as a pump.
Skeletal Muscle
Skeletal muscles act not only to produce movement but also to stop movement, such as resisting gravity to maintain posture. Small, constant adjustments of the skeletal muscles are needed to hold a body upright or balanced in any position. Muscles also prevent excess movement of the bones and joints, maintaining skeletal stability and preventing skeletal structure damage or deformation.
Skeletal muscles are located throughout the body at the openings of internal tracts to control the movement of various substances. These muscles allow functions, such as swallowing, urination, and defecation, to be under voluntary control. Skeletal muscles also protect internal organs (particularly abdominal and pelvic organs) by acting as an external barrier or shield to external trauma and by supporting the weight of the organs.
Skeletal muscles contribute to the maintenance of homeostasis in the body by generating heat. This heat is very noticeable during exercise, when sustained muscle movement causes body temperature to rise, and in cases of extreme cold, when shivering produces random skeletal muscle contractions to generate heat.
Concept Check
- Compare and contrast the 3 types of muscles tissues.
- Where in the body do you find each of the muscle types?
Physiology (Function) of the Muscular System
The main function of the muscular system is to assist with movement. Muscles work as antagonistic pairs. As one muscle contracts, the other muscle relaxes. This contraction pulls on
the bones and assists with movement. Contraction is the shortening of the muscle fibers while relaxation lengthens the fibers. This sequence of relaxation and contraction is influenced by the nervous system.
Muscles also work to keep the posture of the body. This is done through muscle contraction where the trunk is kept straight either when sitting or standing.
Media 14.2 Review of joint movements with Dr. Mike. Copyright 2021, Dr. Matt & Dr. Mike.
ACTION |
MEANING |
| flexion | Decreasing the angle between two bones; bending a limb. |
| extension | Increasing the angle between two bones; straightening out a limb. |
| abduction | Movement away from the midline of the body |
| adduction | Movement toward the midline of the body |
| rotation | Circular movement around an axis (central point). Internal rotation is toward the center of the body and external rotation is away from the center of the body. |
| dorsiflexion | Decreasing the angle of the ankle join so that the foot moves upward, toward the knee or ceiling. This is the opposite movement of stepping on the gas pedal when driving a car. |
| plantar flexion | Motion that moves the foot downward toward the ground as when pointing the toes or stepping on the gas pedal. Plant/o means sole of the foot. |
| supination | As applied to the hand and forearm, where the elbow is bent, the act of turning the palm up. As applied to the foot, it is outward roll of the foot/ankle during normal motion. |
| pronation | As applied to the hand and forearm, where the elbow is bent, the act of turning the palm down. As applied to the foot, it is inward roll of the foot/ankle during normal motion. |
Naming of Muscles
There are many nomenclatures for naming muscles. Some of these include:
- divisions - biceps, triceps, quadriceps
- size - maximus (largest), minimus (smallest)
- shape - deltoid (triangular), trapezious (trapezoid)
- action - flexor (to flex), adductor (towards midline of body)
Muscular System Medical Abbreviations
Common Diseases and Disorders
Muscular Dystrophy
Muscular dystrophies are rare inherited diseases that weaken muscles, decreasing the individual's mobility. There are several kinds of muscular dystrophy that affect different muscle groups and symptoms develop at different ages (Centers for Disease Control and Prevention, 2020). The most common kind of muscular dystrophy is Duchenne/Becker muscular dystrophy (DMD/BMD). This disease primarily effects boys and symptoms may include frequent falls and trouble keeping up with peers. Since all muscles are affected, the person will eventually require a wheelchair and assistance with breathing (Muscular Dystrophy Association, 2021). To learn more please visit the Centers for Disease Control and Prevention muscular dystrophy webpage.
Cerebral Palsy
Cerebral Palsy (CP) is caused by an interruption to the normal development of a person's brain leading to weakness with muscles. Depending on the area of the brain that is affected, signs and symptoms will vary in the type and severity between individuals. Balance and coordination are often challenging due the inability to control muscles (Centers for Disease Control and Prevention, 2020). To learn more about Cerebral palsy please visit the Centers for Disease Control and Prevention.
Carpal Tunnel Syndrome
Carpal tunnel syndrome may present with pain, numbness or weakness to the hand(s) caused by pressure on the median nerve. Some causes for this pressure are work related such as keyboarding with improper body mechanics, illness such as arthritis, and even pregnancy (National Institute of Neurological Disorders and Stroke, 2020). To learn more, visit the National Institute of Neurological Disorders and Stroke webpage.
Paralysis
- Paresis - a partial paralysis wherein there is still some control of the muscles
- Paraplegia - paralysis that affects both legs and lower part of the body.
- Quadriplegia - affects both arms, both legs and sometimes from the neck down
- Hemiplegia - affects one side of the body. For example, the arm and leg on the same side of the body (Cleveland Clinic, 2017)
To learn more about paralysis, please visit the Cleveland Clinic's Paralysis information web page.
Sprain and Strain
A sprain is an injury to a joint whereby a ligament is stretched or torn.
A strain is an injury to a muscle whereby a tendon is stretched or torn.
Diagnostic Procedures
Electromyography (EMG) is a procedure that assesses the function of nerve cells that control muscles. Electrodes, either attached to the skin or inserted into the muscle, allow for the recording of electrical impulses. EMG can identify functional problems with the peripheral nerves, muscles, or with the signals between the nerves and the muscles. This is just one test in a series of tests that assist in the diagnosis of neuromuscular disorders (Mayo Clinic Staff, 2019). To learn more, please visit the Mayo Clinic's Electromyography webpage.
Magnetic Resonance Imaging (MRI) (Fig 14.4) is a test that uses radio frequency waves and a magnetic field to produce clear images that aid in the diagnosis of a wide range of conditions (National Institute of Biomedical Imaging and Bioengineering, n.d.). Leung (2017) notes that there has been increased clinical use in using MRI for the treatment and monitoring of muscular disorders due to the high-quality MRI images that distinguish skeletal muscles from fat (para. 4). To learn more, please visit the National Institute of Biomedical Imaging and Bioengineering MRI webpage.

Range of Motion Testing is a diagnostic procedures used to determine the amount of movement around a specific joint.
Medical Terminology in Context
Medical Specialties Related to Muscular System
Orthopedic Surgeon
Orthopedic Surgeons are medical doctors who complete specialized training in the prevention, diagnosis, treatment and surgery of disorders and diseases related to the musculoskeletal systems (American Academy of Orthopaedic Surgeons, 2021). For more details please visit the American Academy of Orthopaedic Surgeons's page on Orthopaedic Surgeons.
Neurologist
Neurologists are medical doctors who complete an additional specialized training in the prevention, diagnosis, and treatment of disorders and conditions related to the brain, spinal cord, nerves and muscles (American Academy of Neurology, 2021). For more details visit the American Academy of Neurology's webpage.
Kinesiologist
Kinesiologists are regulated health-care professionals with a degree in kinesiology or related discipline. Kinesiologists work in a variety of settings that assist people with pain management, injury prevention, and health promotion through biomechanics (American Kinesiology Association, 2021). To explore career options for kinesiologists, visit the American Kinesiology Association's Career Center webpage. To learn more about kinesiologists and careers in this field, visit the Zippia Kinesiologist Overview webpage.
Occupational Therapist
Occupational therapist helps people across the lifespan to do the things they want and need to do through the therapeutic use of daily activities (occupations). Occupational therapy practitioners enable people of all ages to live life to its fullest by helping them promote health, and prevent—or live better with—injury, illness, or disability. To learn more please visit the American Occupational Therapy Association webpage.
Certified Occupational Therapist Assistant
Certified occupational therapist assistants and aides help patients develop, recover, improve, as well as maintain the skills needed for daily living and working. To learn more please visit the Occupational Outlook Handbook: Occupational Therapy Assistants and Aides.
Physical Therapist
Physical therapists help people to maximize their quality of life. They work with people of all ages and abilities, and in a variety of settings. They help people rehabilitate from devastating injuries, manage chronic conditions, avoid surgery and prescription drugs, and create healthy habits. To learn more please visit: American Physical Therapy Association
Physical Therapist Assistant
Assist physical therapists in providing physical therapy treatments and procedures. May, in accordance with state laws, assist in the development of treatment plans, carry out routine functions, document the progress of treatment, and modify specific treatments in accordance with patient status and within the scope of treatment plans established by a physical therapist. Generally requires formal training. To learn more please visit: Physical Therapist Assistants
Test Yourself
References
American Academy of Neurology. (2021). What is a neurologist? https://www.aan.com/tools-and-resources/medical-students/careers-in-neurology/what-is-a-neurologist/
American Academy of Orthopaedic Surgeons. (2021). Orthopaedic Surgeons: Restoring mobility and keeping our nation in motion. https://www.aaos.org/about/what-is-an-orthopaedic-surgeon/
American Kinesiology Association. (2021). Career Center. https://www.americankinesiology.org/SubPages/Pages/Careers%20In%20Kinesiology#rn
American Occupational Therapy Association. (2021).What is Occupational Therapy. https://www.aota.org/conference-events/otmonth/what-is-ot.aspx
American Physical Therapy Association. (2021). Careers in Physical Therapy. https://www.apta.org/your-career/careers-in-physical-therapy
Centers for Disease Control and Prevention. (2020). What is cerebral palsy? CDC. https://www.cdc.gov/ncbddd/cp/facts.html
Centers for Disease Control and Prevention. (2020). What is muscular dystrophy? CDC. https://www.cdc.gov/ncbddd/musculardystrophy/facts.html
[CrashCourse]. (2015, July 15). Muscles, part 2 - organismal level: Crash course A&P #22 [Video]. YouTube. https://youtu.be/I80Xx7pA9hQ
Leung, J. (2016, November 25). Magnetic resonance imaging patterns of muscle involvement in genetic muscle diseases: a systematic review. Journal of Neurology, 264(7), 1320-1333. https://dx.doi.org/10.1007%2Fs00415-016-8350-6
Mayo Clinic Staff. (2019, May 21). Electromyography (EMG). Mayo Clinic Patient Care and Information. https://www.mayoclinic.org/tests-procedures/emg/about/pac-20393913
Muscular Dystrophy Association. (2021). Duchenne Muscular Dystrophy (DMD). https://www.mda.org/disease/duchenne-muscular-dystrophy
National Institute of Biomedical Imaging and Bioengineering. (n.d.) Magnetic Resonance Imaging (MRI). National Institutes of Health. https://www.nibib.nih.gov/science-education/science-topics/magnetic-resonance-imaging-mri
National Institute of Neurological Disorders and Stroke. (2020). Carpal Tunnel Syndrome Fact Sheet. National Institutes of Health. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Carpal-Tunnel-Syndrome-Fact-Sheet
Occupational Therapy Assistants and Aides. (Sept 2021). Occupational Outlook Handbook. https://www.bls.gov/ooh/healthcare/occupational-therapy-assistants-and-aides.htm
U.S. Bureau of Labor Statistics. (2021). Occupational Therapists. https://www.bls.gov/ooh/healthcare/physical-therapists.htm#tab-1
U.S. Bureau of Labor Statistics. (2021). Physical Therapist Assistants. https://www.bls.gov/oes/current/oes312021.htm#nat
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.
Conservation of the body core heat results in the skin actually freezing
A painful condition in children where bones are misshapen due to a lack of calcium, causing bow leggedness
WTCS Learning Objectives
-
- Apply the rules of medical language to build, analyze, spell, pronounce, abbreviate, and define terms as they relate to the sensory system
- Identify meanings of key word components of the sensory system
- Categorize diagnostic, therapeutic, procedural or anatomic terms related to the sensory system
- Use terms related to the sensory system
- Use terms related to the diseases and disorders of the sensory system
Sensory System Word Parts
Click on prefixes, combining forms, and suffixes to reveal a list of word parts to memorize for the Sensory System.
Introduction to the Sensory Systems
Ask anyone what the senses are, and they are likely to list the five major senses as taste, smell, touch, hearing, and sight. However, these are not all of the senses. The most obvious omission from this list is balance. Touch can be further subdivided into pressure, vibration, stretch, and hair-follicle position, on the basis of the type of mechanoreceptors that perceive these touch sensations. Other overlooked senses include temperature perception by thermoreceptors and pain perception by nociceptors.
Within the realm of physiology, senses can be classified as either general or special. A general sense is one that is distributed throughout the body and has receptor cells within the structures of other organs. Mechanoreceptors in the skin, muscles, or the walls of blood vessels are examples of this type. General senses often contribute to the sense of touch, as described above, or to proprioception and kinesthesia , or to a visceral sense, which is most important to autonomic functions. A special sense is one that has a specific organ devoted to it, namely the eye, inner ear, tongue, or nose. The figure below shows the series of events that lead to stimulation of a sense organ.

Gustation (Taste) and Olfaction (Smell)
Watch this video:
Media 15.1 Taste & Smell: Crash Course A&P #16 [Online video]. Copyright 2015 from CrashCourse.
Sensory System Medical Terms
Gustation (Taste)
Gustation is the special sense associated with the tongue. The surface of the tongue, along with the rest of the oral cavity, is lined by a stratified squamous epithelium. Raised bumps called papillae contain the structures for gustatory transduction. There are four types of papillae, based on their appearance:
- circumvallate
- foliate
- filiform
- fungiform
Within the structure of the papillae are taste buds that contain specialized gustatory receptor cells for the transduction of taste stimuli. These receptor cells are sensitive to the chemicals contained within foods that are ingested, and they release neurotransmitters based on the amount of the chemical in the food. Neurotransmitters from the gustatory cells can activate sensory neurons in the facial, glossopharyngeal, and vagus cranial nerves.
Only a few recognized submodalities exist within the sense of taste, or gustation. Until recently, only four tastes were recognized: sweet, salty, sour, and bitter. Research at the turn of the 20th century led to recognition of the fifth taste, umami, during the mid-1980s. Very recent research has suggested that there may also be a sixth taste for fats, or lipids.
Olfaction (Smell)
Concept Check
- Which parts of the brain are active with recording and associating scents with memories and emotions?
- Recall and list the four types of papillae (taste buds) found on the tongue.
Audition (Hearing), Equilibrium (Balance), and Somatosensation (Touch)
Watch this video:
Media 15.2 Hearing & Balance: Crash Course A&P #17 [Online video]. Copyright 2015 by CrashCourse.
Audition (Hearing)
Hearing, or audition, is the transduction of sound waves into a neural signal that is made possible by the structures of the ear (see Figure 15.2).
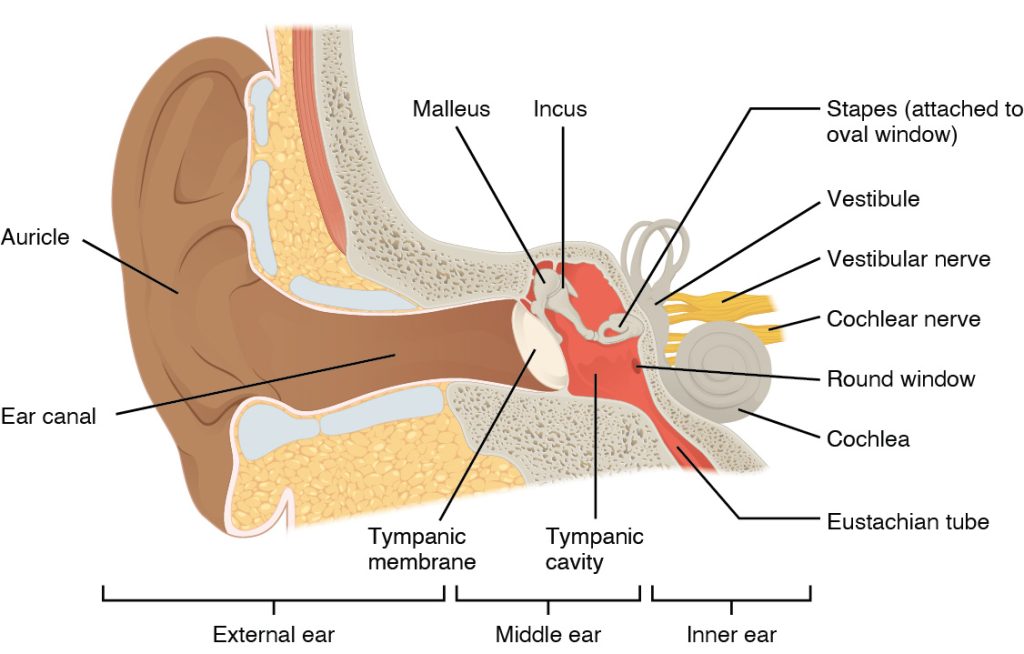
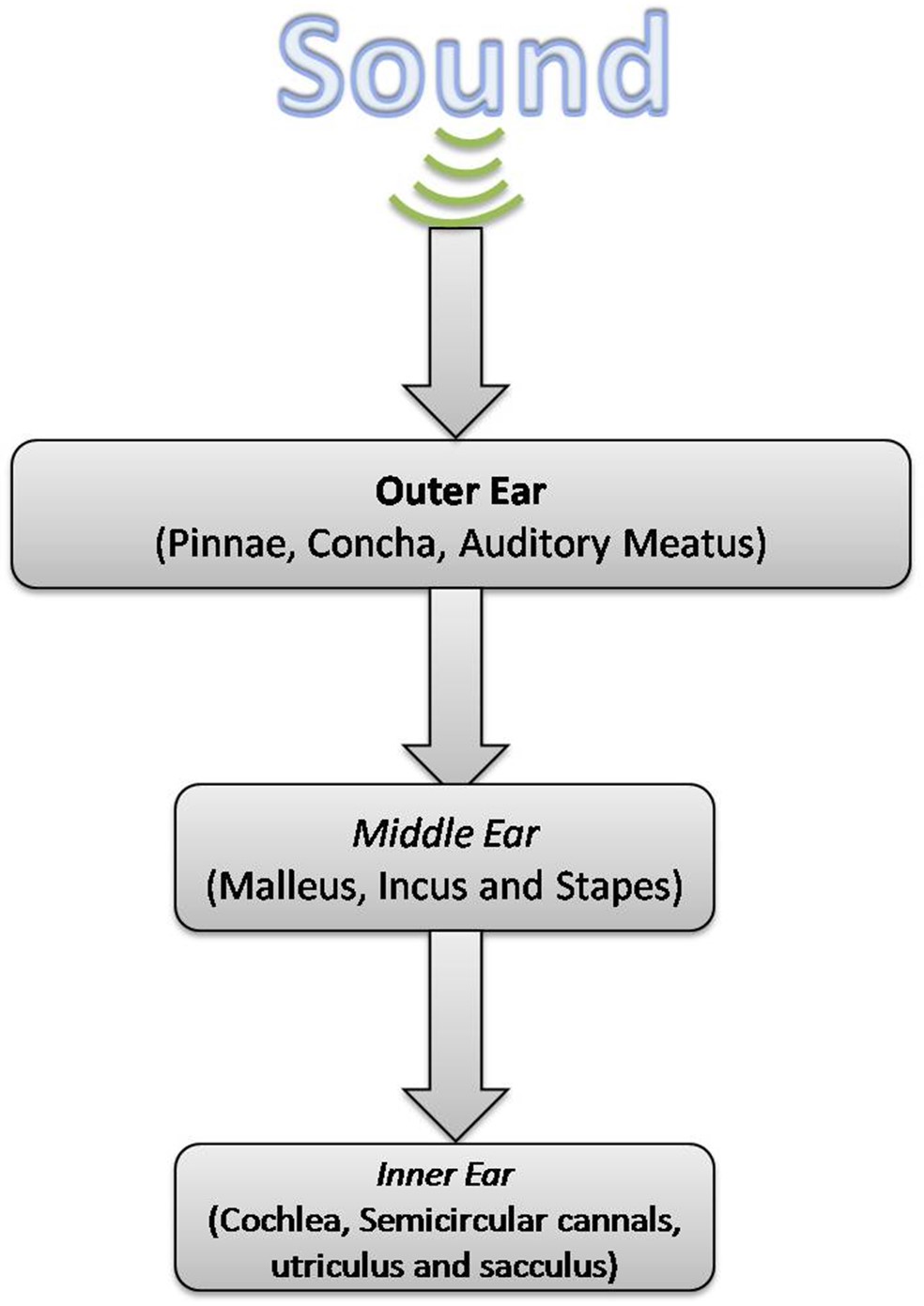
- The external ear consists of the auricle sometimes referred to as the pinna, ear canal, and tympanic membrane.
- The C-shaped curves of the auricle direct sound waves toward the auditory canal. The canal enters the skull through the external auditory meatus of the temporal bone. At the end of the auditory canal is the tympanic membrane, which vibrates after it is struck by sound waves.
- The middle ear consists of the ossicles, oval window, and tympanic membrane.
- The three ossicles are the malleus, incus, and stapes, which are Latin names that roughly translate to hammer, anvil, and stirrup. The malleus is attached to the tympanic membrane and articulates with the incus. The incus, in turn, articulates with the stapes. The stapes is then attached to the inner ear, where the sound waves will be transduced into a neural signal. Vibrations of the ossicles travel through the oval window, moving fluid in a wave-like motion. The frequency of the fluid waves match the frequencies of the sound waves. The middle ear is connected to the pharynx through the Eustachian tube, which helps equilibrate air pressure across the tympanic membrane. The tube is normally closed but will pop open when the muscles of the pharynx contract during swallowing or yawning.
- The inner ear is often described as a bony labyrinth, as it is composed of a series of canals embedded within the temporal bone.
- It consists of the cochlea that is responsible for hearing and the vestibule that is responsible for balance. The neural signals from these two regions are relayed to the brain stem through separate fiber bundles. However, these two distinct bundles travel together from the inner ear to the brain stem as the vestibulocochlear nerve. Sound is transduced into neural signals within the cochlear region of the inner ear, which contains the sensory neurons of the spiral ganglia. These ganglia are located within the spiral-shaped cochlea of the inner ear. The cochlea is attached to the stapes through the oval window.
The image below is a cross-sectional view of the cochlea that shows the scala vestibuli and scala tympani run along both sides of the cochlear duct (see Figure 15.4). The cochlear duct contains several organs of Corti, which tranduce the wave motion of the two scala into neural signals. The organs of Corti lie on top of the basilar membrane, which is the side of the cochlear duct located between the organs of Corti and the scala tympani. As the fluid waves move through the scala vestibuli and scala tympani, the basilar membrane moves at a specific spot, depending on the frequency of the waves. Higher frequency waves move the region of the basilar membrane that is close to the base of the cochlea. Lower frequency waves move the region of the basilar membrane that is near the tip of the cochlea.
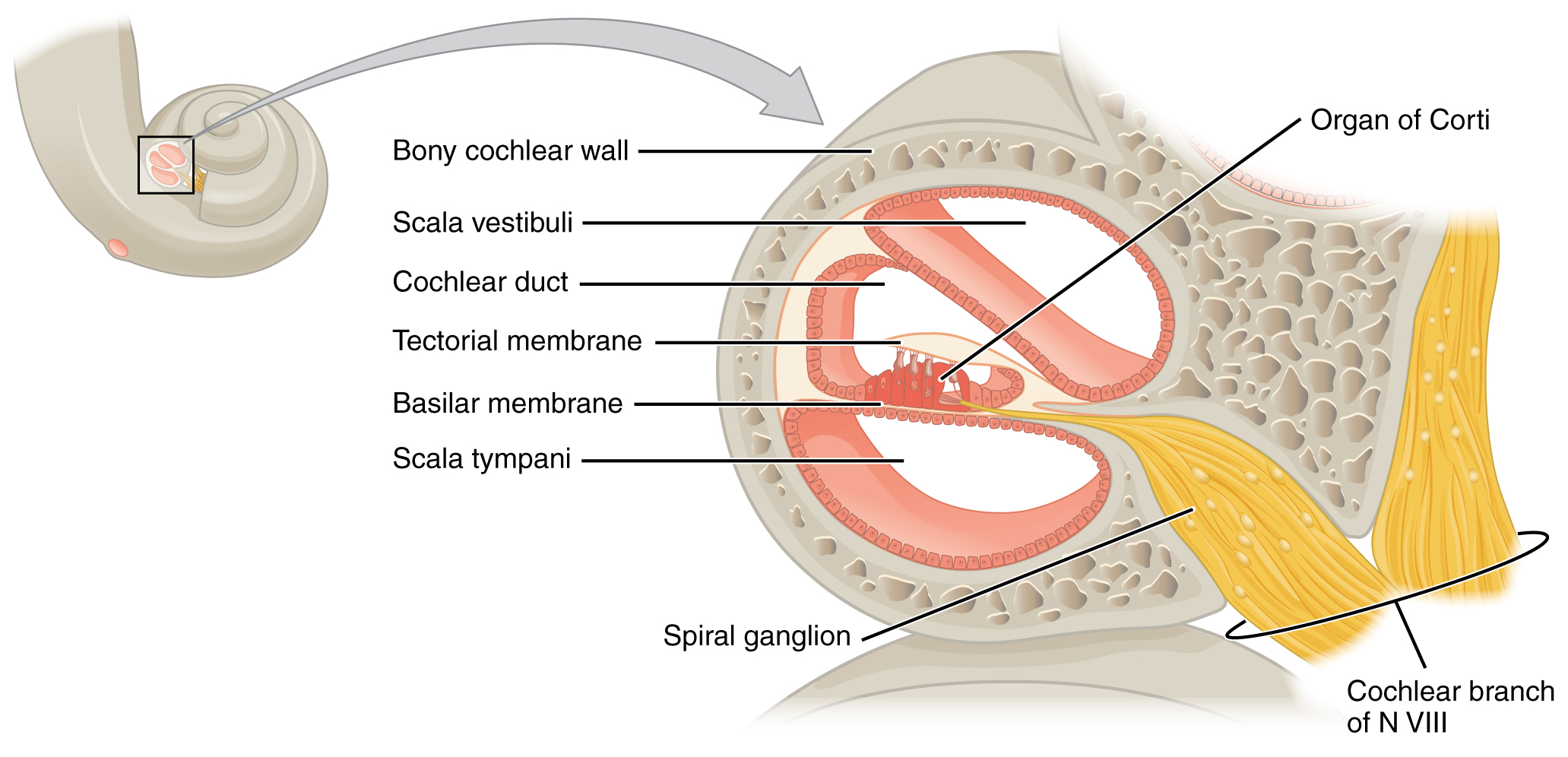
The cochlea encodes auditory stimuli for frequencies between 20 and 20,000 Hz, which is the range of sound that human ears can detect. The unit of Hertz measures the frequency of sound waves in terms of cycles produced per second. Frequencies as low as 20 Hz are detected by hair cells at the apex, or tip, of the cochlea. Frequencies in the higher ranges of 20 KHz are encoded by hair cells at the base of the cochlea, close to the round and oval windows. Most auditory stimuli contain a mixture of sounds at a variety of frequencies and intensities (represented by the amplitude of the sound wave). The hair cells along the length of the cochlear duct, which are each sensitive to a particular frequency, allow the cochlea to separate auditory stimuli by frequency, just as a prism separates visible light into its component colors. To learn more about hearing and the cochlea, watch this Medline Plus video.
Equilibrium (Balance)
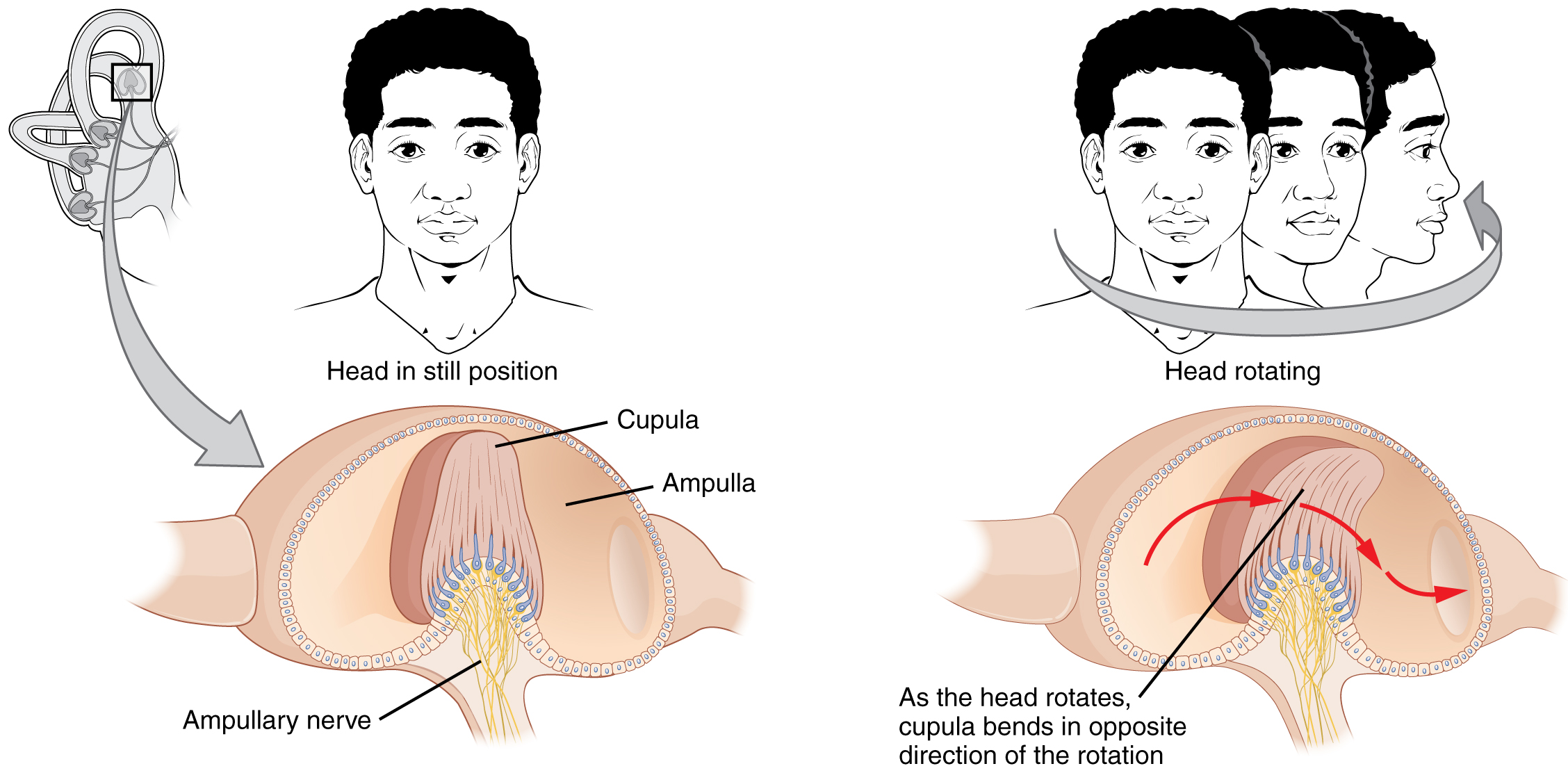
Somatosensation (Touch)
Somatosensation is considered a general sense, as opposed to the special senses discussed in this section. Somatosensation is the group of sensory modalities that are associated with touch, proprioception, and interoception. These modalities include pressure, vibration, light touch, tickle, itch, temperature, pain, proprioception, and kinesthesia. This means that its receptors are not associated with a specialized organ, but are instead spread throughout the body in a variety of organs. Many of the somatosensory receptors are located in the skin, but receptors are also found in muscles, tendons, joint capsules, ligaments, and in the walls of visceral organs.
The two types of somatosensory signals that are transduced by free nerve endings are pain and temperature. Temperature receptors are stimulated when local temperatures differ from body temperature. Some thermoreceptors are sensitive to just cold and others to just heat. Nociception is the sensation of potentially damaging stimuli. Mechanical, chemical, or thermal stimuli beyond a set threshold will elicit painful sensations. Stressed or damaged tissues release chemicals that activate receptor proteins in the nociceptors.
Concept Check
- What structure exists within the ear to assist with maintaining equilibrium?
- What are the medical terms used to describe the sense of taste and touch?
Ear Anatomy Labeling Activity
Vision (Sight)
Watch this video:
Media 15.3 Vision: Crash Course A&P #18 [Online video]. Copyright 2015 by CrashCourse.
Vision is the special sense of sight that is based on the transduction of light stimuli received through the eyes. The eyes are located within either orbit in the skull. The bony orbits surround the eyeballs, protecting them and anchoring the soft tissues of the eye (see Figure 15.6). The eyelids, with lashes at their leading edges, help to protect the eye from abrasions by blocking particles that may land on the surface of the eye.
The inner surface of each lid is a thin membrane known as the palpebral conjunctiva. The conjunctiva extends over the sclera, connecting the eyelids to the eyeball. Tears are produced by the lacrimal gland, located beneath the lateral edges of the nose. Tears produced by this gland flow through the lacrimal duct to the medial corner of the eye, where the tears flow over the conjunctiva, washing away foreign particles.
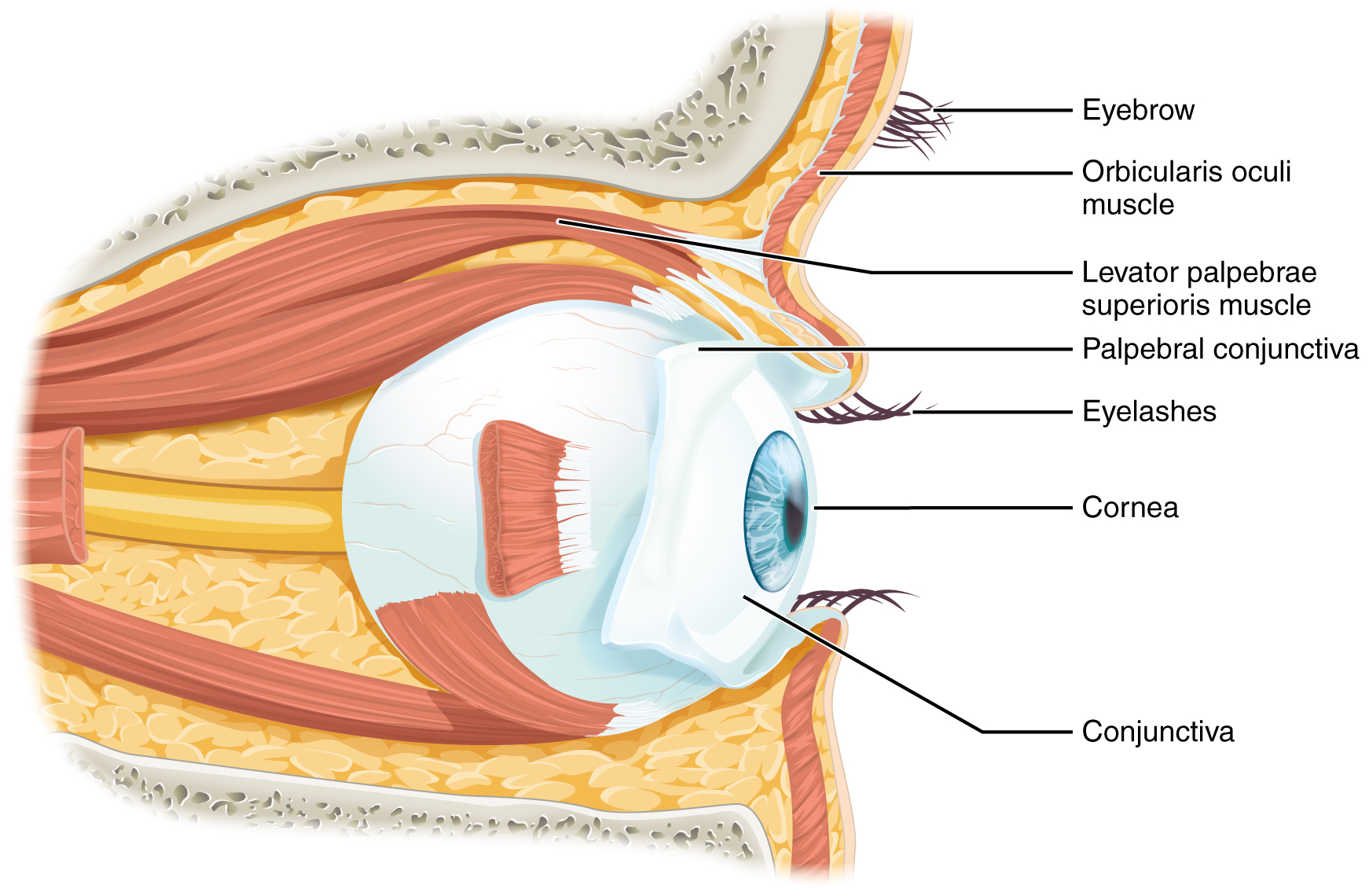
Movement of the eye within the orbit is accomplished by the contraction of six extraocular muscles that originate from the bones of the orbit and insert into the surface of the eyeball. Four of the muscles are arranged at the cardinal points around the eye and are named for those locations. They are the:
- superior rectus
- medial rectus
- inferior rectus
- lateral rectus.
When each of these muscles contract, the eye moves toward the contracting muscle. For example, when the superior rectus contracts, the eye rotates to look up.
The eye itself is a hollow sphere composed of three layers of tissue.
- The outermost layer is the fibrous tunic, which includes the white sclera and clear cornea. The sclera accounts for five sixths of the surface of the eye, most of which is not visible, though humans are unique compared with many other species in having so much of the “white of the eye” visible (see Figure 15.7). The transparent cornea covers the anterior tip of the eye and allows light to enter the eye.
- The middle layer of the eye is the vascular tunic, which is mostly composed of the choroid, ciliary body, and iris. The choroid is a layer of highly vascularized connective tissue that provides a blood supply to the eyeball. The choroid is posterior to the ciliary body, a muscular structure that is attached to the lens by zonule fibers. These two structures bend the lens, allowing it to focus light on the back of the eye. Overlaying the ciliary body, and visible in the anterior eye, is the iris—the colored part of the eye. The iris is a smooth muscle that opens or closes the pupil, which is the hole at the center of the eye that allows light to enter. The iris constricts the pupil in response to bright light and dilates the pupil in response to dim light.
- The innermost layer of the eye is the neural tunic, or retina, which contains the nervous tissue responsible for photoreception.
The eye is also divided into two cavities:
- The anterior cavity
- The anterior cavity is the space between the cornea and lens, including the iris and ciliary body. It is filled with a watery fluid called the aqueous humor.
- The posterior cavity
- The posterior cavity is the space behind the lens that extends to the posterior side of the interior eyeball, where the retina is located. The posterior cavity is filled with a more viscous fluid called the vitreous humor.
The retina is composed of several layers and contains specialized cells for the initial processing of visual stimuli. The photoreceptors (rods and cones) change their membrane potential when stimulated by light energy. The change in membrane potential alters the amount of neurotransmitter that the photoreceptor cells release onto bipolar cells in the outer synaptic layer. It is the bipolar cell in the retina that connects a photoreceptor to a retinal ganglion cell (RGC) in the inner synaptic layer. There, amacrine cells additionally contribute to retinal processing before an action potential is produced by the RGC. The axons of RGCs, which lie at the innermost layer of the retina, collect at the optic disc and leave the eye at the optic nerve (see Figure 15.7). Because these axons pass through the retina, there are no photoreceptors at the very back of the eye, where the optic nerve begins. This creates a “blind spot” in the retina, and a corresponding blind spot in our visual field.
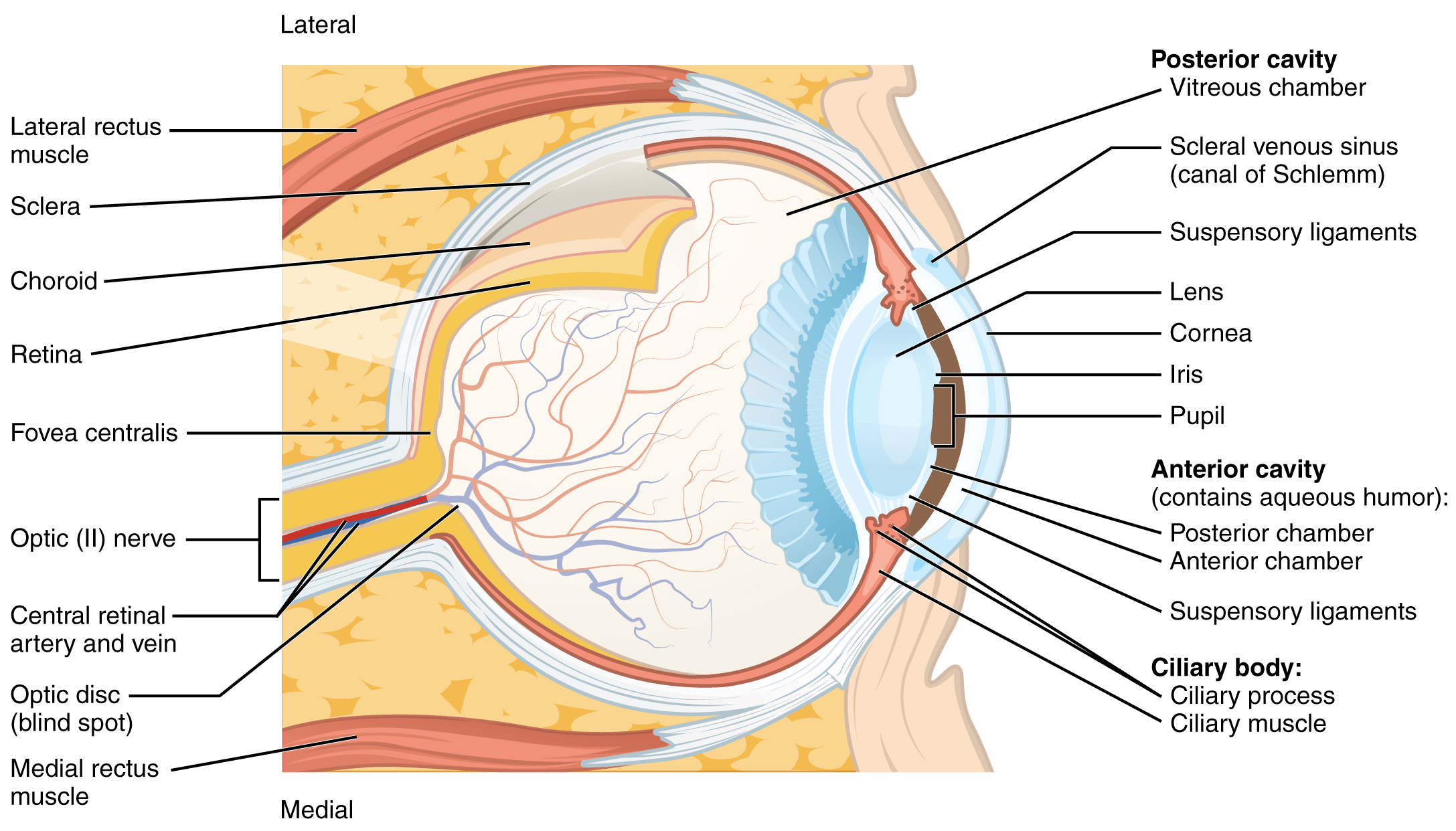
Photoreceptors in the retina (rods and cones) are located behind the axons, RGCs, bipolar cells, and retinal blood vessels. A significant amount of light is absorbed by these structures before the light reaches the photoreceptor cells. At the exact center of the retina is a small area known as the fovea. At the fovea, the retina lacks the supporting cells and blood vessels, and only contains photoreceptors. Therefore, visual acuity, is greatest at the fovea. This is because the fovea is where the least amount of incoming light is absorbed by other retinal structures (see Figure 15.7). As one moves in either direction from this central point of the retina, visual acuity drops significantly.
Example: Visual Acuity (VA) between the fovea and peripheral retina.
There are three types of cone opsins, that are sensitive to different wavelengths of light and provide us with color vision. By comparing the activity of the three different cones, the brain can extract color information from visual stimuli (see Figure 15.8). For example, a bright blue light that has a wavelength of approximately 450 nm would activate the “red” cones minimally, the “green” cones marginally, and the “blue” cones predominantly. The relative activation of the three different cones is calculated by the brain, which perceives the color as blue. However, cones cannot react to low-intensity light, and rods do not sense the color of light. Therefore, our low-light vision is, in essence, in grayscale. In other words, in a dark room, everything appears as a shade of gray. If you think that you can see colors in the dark, it is most likely because your brain knows what color something is and is relying on that memory.
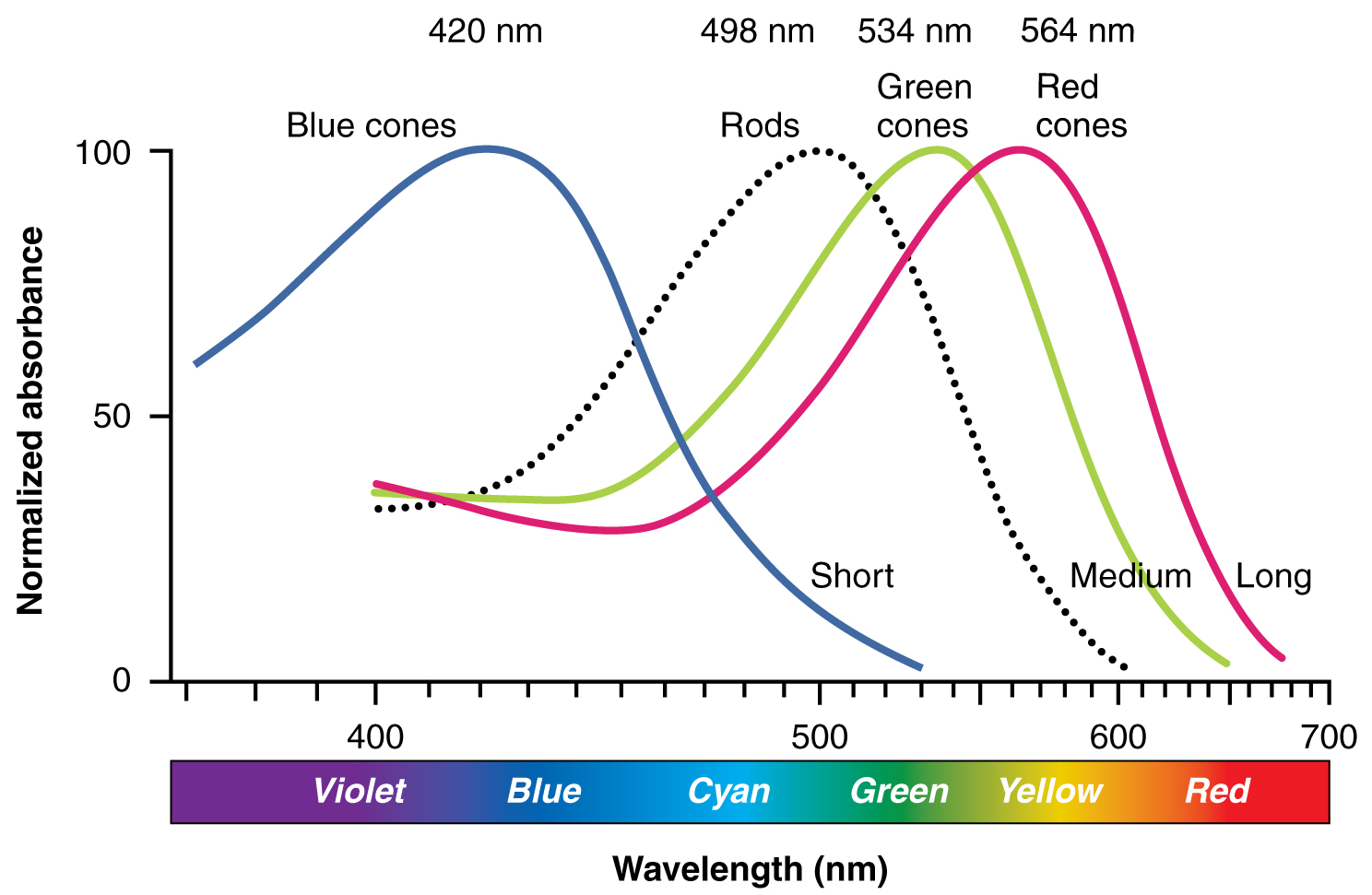
Sensory System Medical Terms Not Easily Broken Into Word Parts
Anatomy Labeling Activity
Sensory System Terms not Easily Broken into Word Parts
Common Abbreviations for the Sensory System
Diseases and Disorders of the Sensory Systems
Olfactory Diseases and Disorders
Anosmia
Blunt force trauma to the face, such as that common in many car accidents, can lead to the loss of the olfactory nerve, and subsequently, loss of the sense of smell. This condition is known as anosmia. When the frontal lobe of the brain moves relative to the ethmoid bone, the olfactory tract axons may be sheared apart. Professional fighters often experience anosmia because of repeated trauma to face and head. In addition, certain pharmaceuticals, such as antibiotics, can cause anosmia by killing all the olfactory neurons at once. If no axons are in place within the olfactory nerve, then the axons from newly formed olfactory neurons have no guide to lead them to their connections within the olfactory bulb. There are temporary causes of anosmia, as well, such as those caused by inflammatory responses related to respiratory infections or allergies.
Loss of the sense of smell can result in food tasting bland. A person with an impaired sense of smell may require additional spice and seasoning levels for food to be tasted. Anosmia may also be related to some presentations of mild depression, because the loss of enjoyment of food may lead to a general sense of despair. The ability of olfactory neurons to replace themselves decreases with age, leading to age-related anosmia. This explains why some elderly people salt their food more than younger people do. However, this increased sodium intake can increase blood volume and blood pressure, increasing the risk of cardiovascular diseases in the elderly (Betts, et al., 2021).
Ears, Nose, and Throat Diseases and Disorders
Otitis Media
Otitis Media is known as inflammation of the middle ear canal that involves the eardrum. It is commonly seen in younger children due to bacterial and viral infections. Symptoms include possible fever, cough and cold symptoms, hearing loss, irritability and otalgia. Treatment involves symptomatic control as well as antibiotic (Amoxicillin) use if necessary (Danishyar and Ashurst 2021). To learn more about otitis media visit this webpage from the National Center for Biotechnology Information bookshelf.
Otitis Externa
Otitis Externa is inflammation of the external ear canal and is known as swimmer’s ear because it is associated with its exposure to water. Its clinical presentation and management are the same as otitis media (Piercefield, et al., 2011). To learn more about otitis externa review this website from the Centers for Disease Control and Prevention.
Conductive Hearing Loss
Hearing loss occurs when something disrupts sound through the mid and outer ear, such as physical damage to the ear drum (perforation). Hearing loss can be managed with pharmacotherapy, surgery or a combination of the two (Centers for Disease Control and Prevention, 2020).
Sensorineural Hearing Loss
This hearing loss results from damage to the neural structures. Tumors as well as exposure to loud noises (acute/chronic) can lead to this type of hearing loss (Centers for Disease Control and Prevention, 2020). To learn more about sensorineural hearing loss review the Centers for Disease Control and Prevention's web page about sensorineural hearing loss.
Tinnitus
Tinnitus is a condition of perceived ringing in the ears. Tinnitus can be caused by many underlying health conditions, including inflammation or obstruction within the middle ear (American Tinnitus Association, 2019). To hear what tinnitus can sound like, visit the American Tinnitus Association's webpage.
Otosclerosis
This is hardening of the ear due to new bone formation of the inner ear ossicles. Its etiology is of idiopathic or hereditary origin. Clinical features are consistent with that of conductive hearing loss. Treatment for mild otosclerosis involves use of a hearing aid, while more severe otosclerosis is treated with a stapedectomy surgery (National Institute on Deafness and Other Communication Disorders, 2018). To learn more visit the National Institute on Deafness and Other Communication Disorders webpage on Otosclerosis.
Rhinitis
Is inflammation of the nasal cavity mucosal lining which can lead to congestion and rhinorrhea (runny nose). The causes are due to allergic reactions as well as viruses. Treatment regimens include symptomatic management, saline sprays and oral antihistamines (Naclerio, Bachert, & Baraniuk, 2010).
Eye Diseases and Disorders
Blindness
The term “blindness” may cover a broad spectrum of visual disability such as the inability to see because of injury, disease, or a congenital condition. The parameters for legal blindness are visual field is 20 degrees or narrower and/or visual acuity is 20/200 or less in the best seeing eye even after correction. Many of the conditions described below lead to visual disability, low vision, and legal blindness (Lee and Mesfin, 2020). To learn more about blindness visit the National Library of Medicine's webpage.
Cataract
A cataract is a clouding of the normally clear lens of your eye. For people who have cataracts, it's like seeing through cloudy lenses or windows. The lens of the eye loses its flexibility due to the aging process leading in some cases to senile cataracts. Infants sometime are born with congenital cataracts. Treatment usually involves surgery to remove the clouding of the lens (Mayo Clinic Staff, 2018). To learn more, visit the Mayo Clinic's web page about cataracts.
Conjunctivitis
This is a condition involving inflammation of the conjunctiva. Its common causes are due to allergens, chemicals, foreign objects, as well as bacterial and viral pathogens. The cause of conjunctivitis determines if it is transmissible from one individual to another. Pink eye caused by the adenovirus for example, is highly contagious compared to pollen which is not. Management involves treating the underlying cause of the conjunctivitis (Centers for Disease Control and Prevention, 2019). To learn more about conjunctivitis please visit the Centers for Disease Control and Prevention's web page about conjunctivitis.
Diabetic Retinopathy
This is a disease of the retina caused by diabetes mellitus. The retinal veins dilate leading to swelling as fluid leaks from blood vessels into the retina. It is estimated that 20% of newly diagnosed diabetics suffer from diabetic retinopathy (American Optometric Association, 2020). To learn more visit the American Optometric Association 's website on diabetic retinopathy.
Glaucoma
This disease is part of a group of eye diseases which lead to progressive degeneration of the optic nerve. This, in turn, can lead to loss of nerve tissue that results in gradual irreversible vision loss and potential blindness if not detected and treated early. The most common form of glaucoma is primary open angle glaucoma. This form is associated with elevated pressure caused by a backup of fluid in the eye (National Eye Institute, 2020). To learn more visit the National Eye Institute's webpage about glaucoma.
Macular Degeneration/ Age-related Macular Degeneration (AMD)
Progressive damage of a portion of the retina known as the macula. Severe central vision is lost with peripheral vision retained. This is the leading cause of blindness in Americans over the age of 65 (Centers for Disease Control and Prevention, 2020). To learn more visit the Centers for Disease Control and Prevention webpage on AMD.
Nystagmus
This is condition whereby involuntary repetitive eye movements that make it impossible to fixate on a single object. The condition is often referred to dancing eyes (Dubow, 2020). To learn more information about nystagmus view this website from All About Vision.
Retinal Detachment
This condition occurs when the retina gets pulled away or separated from its normal position. Flashing lights, floaters and what appears to be a grey curtain are all symptoms of a retinal tear, which can lead to a retinal detachment. An ophthalmologist is a retinal specialist who can repair the retinal detachment. If left untreated a retinal detachment could lead to blindness (National Eye Institute, 2020). To learn more visit the National Eye Institute's page on retinal detachment.
Strabismus
This is a condition where the affected eye rotates due to mismatched eye coordination. Each eye is focused differently as described below:
- Estropia: the convergence of one or both eyes medially.
- Extropia: the deviation of one eye laterally.
- Hypertropia: the deviation of one eye superiorly.
- Hypotropia: the deviation of one eye inferiorly.
If not managed, the brain may reject input from one eye resulting in vision loss of the respective eye (amblyopia). Amblyopia is a condition also known as lazy eye which is caused when there is an imbalance of stimuli from the brain to the eyes (one eye receives more than the other).
Medical Terms in Context
Medical Specialties and Procedures Related to the Sensory Systems
Several medical specialties support the sensory systems. An optometrist is an eye specialist that examines and evaluates for ocular pathology and an optometrist prescribes corrective lenses. An ophthalmologist evaluates and manage eye pathology as well as perform surgery. An otorhinolaryngologist (ENT) is a physician that specializes in ears, nose and throat treatment and conditions. An audiologist evaluates and manages individuals with hearing loss.
Ophthalmic Medical Assistant
Ophthalmic Medical Assistants work in ophthalmic and optometric practices and in retail optical settings. Ophthalmic Assistants perform pre-screening and specialty testing, assist with dispensing glasses and contact lenses, and perform office management duties including maintaining patient information and billing and insurance processes.
Ophthalmic Technician
Optometric Technicians work under the supervision of an optometrist or ophthalmologist. Optometric Technicians assist an optometrist during eye exams and other optometric procedures, providing eye health tests and consultations.
Test Yourself
References
American Optometric Association. (2020). Diabetic retinopathy. https://www.aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions/diabetic-retinopathy
American Tinnitus Association. (2019). Understanding the Facts. https://www.ata.org/understanding-facts
CrashCourse. (2015, May 11). Vision: Crash course A&P #18 [Online video]. YouTube. https://www.youtube.com/watch?v=o0DYP-u1rNM
CrashCourse. (2015, APril 27). Taste & smell: Crash course A&P #16 [Online video]. YouTube. https://www.youtube.com/watch?v=mFm3yA1nslE
CrashCourse. (2015, May 4). Hearing & balance: Crash course A&P #17 [Online video]. YouTube. https://www.youtube.com/watch?v=Ie2j7GpC4JU
Centers for Disease Control and Prevention. (2019). Conjunctivitis (pink eye). CDC. https://www.cdc.gov/conjunctivitis/about/causes.html
Centers for Disease Control and Prevention. (2020). Learn about age-related macular degeneration. CDC. https://www.cdc.gov/visionhealth/resources/features/macular-degeneration.html
Centers for Disease Control and Prevention. (2020). Types of hearing loss. CDC. https://www.cdc.gov/ncbddd/hearingloss/types.html
Danishyar A, Ashurst JV. Acute Otitis Media. (Updated 2021 Mar 16). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK470332/
Dubow, B. (2020). Nystagmus: Involuntary eye movements. All About Vision. https://www.allaboutvision.com/conditions/nystagmus.htm
Lee SY, Mesfin FB. Blindness. (Updated 2020 Oct 28). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. https://www.ncbi.nlm.nih.gov/books/NBK448182/
Mayo Clinic Staff. (2018). Cataracts overview. Mayo Clinic Patient Care & Health Information. https://www.mayoclinic.org/diseases-conditions/cataracts/symptoms-causes/syc-20353790
Naclerio, R.M., Bachert, C., & Baraniuk, J.N. (2010). Pathophysiology of nasal congestion. International Journal of General Medicine, 3, 47-57. https://dx.doi.org/10.2147%2Fijgm.s8088
National Institute on Deafness and Other Communication Disorders. (2018). Otosclerosis. National Institutes of Health. https://www.nidcd.nih.gov/health/otosclerosis
National Eye Institute. (2020). Glaucoma. National Institutes of Health. https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/glaucoma
National Eye Institute. (2020). Retinal detachment. National Institutes of Health. https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/retinal-detachment
Piercefield, E.W., Collier, S.A., Hlavsa, M.C., & Beach, M.J. (2011). Estimated burden of acute otitis externa - United States, 2003-2007. CDC Morbidity and Mortality Weekly Report. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6019a2.htm?s_cid=mm6019a2_w
Unless otherwise indicated, this chapter contains material adapted from Anatomy and Physiology (on OpenStax), by Betts, et al. and is used under a a CC BY 4.0 international license. Download and access this book for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.
Specialized cells that produce melanin which is a dark pigment responsible for colouration of skin and hair.
Molecules are transported out of cells. A form of active transport
biological process that results in stable equilibrium
Pertaining to dendrites
abnormal cells in the body dividing uncontrollably.
non cancerous, harmless
Production of cells that can mobilize and establish tumors in other organs of the body
yellow discoloration of the skin
Yellow coloured
abnormal condition of blue (bluish colour, lips and nail beds) caused by deoxygenation.
loss of fluids/water is greater then what is taken in.
pertaining to within the vein
invasion by disease causing organisms
disease causing agents
excision of damaged tissue or foreign object.
collagen-rich skin formed after the process of wound healing that differs from normal skin
formation of a raised or hypertrophic scar
tissue death
pertaining to dermatology
Study of diseases of the skin.
remove by cutting out

