3.1 Careers in Healthcare
Anita Hedlund

Choosing Healthcare as a Career
For those who are considering a career in healthcare, there are many compelling reasons to choose this field over others. Many gravitate toward careers in healthcare due to its mission and values. The healthcare system strives to prevent, diagnose, and treat all manner of disease and illness, and it takes a diverse group of trained professionals in various settings to serve the patients that rely on them.
Many people pursue healthcare careers out of a desire to help others. Changing another person’s life by positively impacting their health is highly fulfilling on both a personal and professional level, and values and traits such as compassion and empathy can be an integral part of serving patients daily. The care a patient receives varies in approach and intensity depending on their needs and health conditions. Patient care can be as personal as helping a patient with daily activities such as bathing, dressing, eating, and walking. Healthcare professionals can save lives, improve health conditions, and support patients in maintaining their health or dying with dignity.
In addition to helping others, there is a great deal of job security in healthcare. Demand for most healthcare roles is increasing as the population ages and expands, and salaries are rising due to this demand. Once a person learns some medical terminology and develops familiarity with healthcare systems and processes, they will have opportunities to advance in responsibility, pursue new interests within healthcare, and continue with further education and training.
This book contains chapters that go into detail about each type of healthcare career, such as nursing, dentistry, pharmacy, physical therapy, office, and administrator positions. In addition, there are chapters on law and ethics in healthcare, applying and interviewing for healthcare jobs, and professionalism in healthcare, among other topics.
Introducing Career Pathways in Healthcare
There are many options for serving others in a healthcare role. Some people have an aversion to dealing with human body fluids, such as blood, but would find fulfillment in an administrative capacity, such as billing or management of health records. Other options include counseling, social work, or another non-direct patient care role. If you know another language, medical interpreting is an in-demand role.
It is important to note that not all care is focused on illness; a critical part of healthcare is disease prevention through wellness promotion. This includes promoting a healthy diet, encouraging regular exercise, and providing education on other lifestyle choices, such as tobacco use. Another element of healthcare with a wellness focus is helping people who are recovering from injury or surgery regain function. Physical or occupational therapists and therapy assistants help these patients strengthen muscles and increase flexibility with rehabilitation exercises. Massage therapists may work in a physical therapy clinic or in a relaxation-focused environment such as a spa. Additionally, some careers might interact with patients in other capacities, such as in radiology, where imaging technicians might perform ultrasounds to monitor progress during pregnancy or perform X-rays to help identify broken bones following an injury.
Some people may prefer the more hands-on applications of medicine. If so, a role in direct patient care may be appropriate. Examples of direct patient care include taking blood pressure, giving injections, bathing, assisting with walking, performing CPR, and working with patients undergoing surgery.
Other people may enjoy specializing in a certain part of the body. For example, those interested in oral health might be drawn to dentistry. Those fascinated by the work of the heart and its associated structures may wish to pursue a career as a nurse in a cardiac intensive care unit, caring for people with heart conditions or those recovering from heart surgery. There are also roles imaging the heart’s blood vessels in cardiac catheterization labs. Those interested in the lungs or breathing may want to help people with issues such as asthma, the need for oxygen therapy, or managing mechanical ventilation for critically ill patients as a respiratory therapist. Alternatively, interest in muscles and bones may lead to professions related to function and injury, such as sports medicine or physical therapy. Someone who is interested in how medication works in the body and enjoys customer service may find a career as a pharmacy technician appealing, as this role involves both aspects.
Healthcare also offers high-adrenaline jobs for those who thrive in fast-paced or intense care roles, such as emergency medical technicians who respond to 911 calls. Working in certain environments, such as an emergency department, can offer busy and challenging shifts interacting with patients who are experiencing cardiac arrest, heart attacks, strokes, or trauma. In healthcare, there is always a specialty where you can explore the subjects that interest you.
Reflection:
Reflect on what has made healthcare an area of interest for you. Was it a personal experience, observing the care of a loved one, watching inspirational caregivers in action, or feeling called to help others? Was it job security, good pay, or flexible schedules? If you were asked in an interview what drew you to healthcare, how would you answer?
Educational Preparation and Licensure

All the careers mentioned thus far are attainable through either a certificate program of 1 month to less than 1 year, or prerequisites plus a specific program of study resulting in a degree. Prerequisites lay a foundation of knowledge that will help the student succeed in the specialized program.
Most healthcare careers require common science prerequisites such as biology, anatomy, physiology, nutrition, and chemistry courses. If a program is an associate’s degree or higher, there will be general college requirements such as English, psychology, communication, and math courses. A two-year program at a community or technical college would earn the graduate an associate’s degree. There are also four-year programs leading to a bachelor’s degree. Bachelor’s degrees are typically part of four-year colleges and universities but are sometimes offered at community and technical colleges if there is an obvious need.
Some careers in healthcare, such as nursing, can be thought of in terms of steps. For example, someone interested in nursing could start as a nursing assistant, which only requires 1 to 3 months of training, providing basic care to patients such as assistance with eating and bathing. In this example, becoming a nursing assistant is “step one” because it allows for someone to begin working in the field quickly. “Step two” might be to pursue licensure as a practical or registered nurse, each with its own programs and prerequisites. Because the previous step provides valuable experience in the field, and each level of education supports the next, there is room for a person to grow within their profession through higher levels of education. The nurse in our example may choose to pursue a bachelor’s, master’s, or even doctoral degree, each its own “step” in this nurse’s professional development. These advanced programs might be undertaken to gain advanced education in public health, become a provider such as a nurse practitioner, learn to be a researcher, or work in higher education as an instructor or professor.
The time it takes to finish an education program can be an important consideration when choosing a field but should not be a barrier. All healthcare settings have opportunities that do not require advanced degrees. Pharmacy and physical or occupational therapy offer entry-level positions as pharmacy technicians and physical or occupational therapy assistants. Typically, these entry-level positions require a two-year associate’s degree. Other positions in these same settings, such as pharmacists or physical therapists, require a doctoral degree, which can take 7 to 8 years of college before being able to care for patients. Most areas in healthcare have varying levels of education for roles that work together as a team to provide care. A good example is a dental office, where a receptionist, a billing specialist, dental assistants, dental hygienists, and dentists all work together with differing educational backgrounds to provide different aspects of the patient’s care.
Education cannot be discussed without mentioning recent, exciting advances in technology. Programs preparing the next generation of healthcare practitioners are using technology to simulate what students will experience in the field. There are now high-fidelity manikins that can talk, cry, and cough. Manikins may even have heart and lung sounds and can be made to have wounds or even changes in blood pressure. Simulation, where learners work in a team to practice managing a specific healthcare issue in a realistic setting, is a valuable learning modality and a major underpinning of today’s programs. In some cases, virtual reality tools are used to allow learners to practice what they would do in certain care scenarios.

Certification and Licensure
Every role that entails direct patient care requires some form of professional credential. The type of credential is unique to a particular healthcare profession. The law regulating the profession determines whether the credential needs to be a license, certification, registration, temporary or limited license, or permit. Usually, documentation from an educational program is submitted to the state or organization, and a fee is collected to provide the certification or license. A license or certification is usually required before a person can practice a healthcare profession. The qualifications for specific professions are set in state law. Additionally, some careers require a national board exam after graduation from an educational program to meet qualifications, such as nursing and respiratory therapy. After successfully passing the exam, a fee is normally paid. For example, as of 2024, a registered nurse in Washington state would pay $138 for their license (Washington State Board of Nursing, 2024). Keep in mind that some licenses restrict eligibility. Some examples of barriers to healthcare licensure include certain felony convictions relating to drugs, abuse of a spouse, abuse of a child, or abuse of the elderly or vulnerable. While some programs may do a background check to ensure that you qualify, it is important to be aware and personally check with programs to ensure you are not disqualified from necessary credentials.
Yearly renewal fees are often required to keep licenses active, and many professions also require ongoing additional training or education over a certain period, such as 1 year or 3 years. This is to make sure people are aware of any changes, such as new laws, scope of practice, new scientific evidence, and advances in technology related to their field.
See Appendix 2 for a link to health professions and the associated fees in Washington state.
Advantages of Employment in Healthcare
Job Security
A major draw to the healthcare field is job security. Healthcare is one of the fastest growing fields due to the increasing number of people who need health services. The U.S. population is projected to grow by almost 17 million by 2030, and as individuals age, their healthcare needs tend to increase. As of 2021, people over 50 make up 36% of the U.S. population (USAFacts, 2023). Regardless of age, diseases such as diabetes and conditions such as hypertension are common, with patients needing health education, screenings, and checkups to maintain their best health. People of all ages need emergency care and preventive health measures, such as immunizations and information about optimal nutrition and exercise, expanding the need for healthcare professionals to provide these important services.
Pay and Salary
Healthcare has some of the highest pay based on level of education compared to other industries. Due to the current shortage of healthcare workers in many roles, there are often hiring bonuses of up to several thousand dollars. Comprehensive healthcare and other benefits, such as retirement savings, are offered in almost all full-time positions and are often available even for part-time workers. If an employee wishes to advance their education, many health organizations offer tuition support for the promise of that employee providing future service with the skills or licensure they earn. This allows healthcare workers to advance further in their field while their organization benefits from the increased level of care their staff can provide.
Learning Activity: Salaries
Salary can be a big part of why someone does or does not choose a profession. Think back to Abeba’s story. If you were going to help Abeba find out more about salaries, where might you go to find that information?
Pretend you are helping Abeba do some research on medical assistants, registered nurses, and dental hygienists in Washington state. Visit the Bureau of Labor Statistics to find out more.
There are two healthcare categories, Healthcare Practitioners and Technical Occupations and Healthcare Support Occupations, which includes dental, medical, nursing, occupational therapy, and physical therapy assistants.
Settings and Schedules
The schedule of a healthcare worker varies depending on the position. Some jobs, such as those in an office or business department, have the traditional eight-hour, five-day-a-week, full-time schedule. Hospital workers such as nursing assistants, nurses, and respiratory therapists often work 12-hour shifts, 3 days a week, which is considered full-time. Typical shifts are 7:00 a.m. to 7:30 p.m. and 7:00 p.m. to 7:30 a.m. Those who work the overnight shift earn extra pay, called a shift differential. Some positions in clinics may offer four 10-hour shifts per week, allowing for 3 days off. Some nurses visit patients in their own homes, which may change how their schedule looks. Emergency workers such as paramedics may work 24-hour shifts that include waiting to respond. There are also part-time and on-call positions in many departments. Working from home is another possibility in some roles, such as a medical coder working with health information, since they are not working with patients directly. Portions of other jobs can be done over the phone or via video conferencing applications such as Zoom or Teams. There are also temporary and short-term contracted positions that may have a higher level of flexibility than others.
One potential downside of healthcare is that hospitals and emergency services must be staffed 24 hours a day every day of the year, including holidays. Many employment contracts also require people to work every other weekend. Although there is often a pay differential for weekend shifts and holiday work, it can mean time away from family on special occasions. Typically, a workplace has a schedule where holidays are rotated among staff. Employees who wish to maintain a religious observance need to communicate with their employer.
Travel
Once a person is trained for certain in-demand roles and gains some experience, there may be opportunities to travel to fill staffing shortages all over the country. These contracts are typically for 3 months and are usually in high-demand professions. Being trained in certain healthcare roles can also create opportunities to work and explore globally, allowing healthcare professionals to develop an understanding of other cultures and languages. Voluntary and paid positions exist with organizations such as the Red Cross and Doctors Without Borders, which send healthcare workers to international destinations to help in a crisis or to offer surgery and other treatment in underserved areas or places where accessing healthcare is difficult. These positions may range from the standard few months to a few years. Groups such as Operation Smile typically go to a region for a few weeks at a time and perform surgeries, such as cleft lip and palate repair, so they need all roles related to surgical care and patient recovery. The surgeries are offered for free or pay-as-able to the community. These travel opportunities are unforgettable and can be life-changing experiences for both the patients and the workers.
Learning Activity: Recruiting in Your Area
Search through a recruiting site or hiring page for a local hospital and take a look at job postings in the healthcare field. Are there a lot of openings in the area where you live? What kind of positions are they trying to fill?
Now, reflect on how your career would be most fulfilling if you have a passion for or find joy in what you do for work. How does this come into balance with the financial and time investment required for your educational program and the salary you will earn when entering the field? Would you be able to fill a need in your community keeping all these factors in mind?
Common Themes and Values Across Careers

Patients First
One critical aspect of caring for others is to put the patient and their loved ones first, also known as patient-centered care. This may seem like an obvious priority, but historically, doctors were seen as having great power and knowledge, and patients followed their recommendations without question, creating opportunities for healthcare professionals to take advantage of patients. NEJM Catalyst (2017) defines patient-centered care as a relationship in which “an individual’s specific health needs and desired health outcomes are the driving force behind all healthcare decisions and quality measurements.” Healthcare professionals using this approach view patients as partners in the pursuit of optimal health, considering not only their physical needs but also how emotional, mental, spiritual, social, and financial factors affect their health.
In addition, patient-centered care is provided with sensitivity and respect for the diversity of human experience, taking into account the patient’s values, preferences, and needs. Healthcare workers must be willing to reflect on and examine their own attitudes about working with patients from different ethnic, cultural, political, and social backgrounds, whose values may differ from their own (Quality and Safety Education for Nurses [QSEN] Institute, 2023).
Values and Ethics
While there are many roles in healthcare, there are some common attributes of those who serve others that will make healthcare a good fit as a career choice. Compassion, empathy, and patience are necessary when spending your working hours in service positions. Values such as honesty, responsibility, and accountability can help to direct an individual’s decision making in the field. Because so many people, from patients to peers, are relying on healthcare professionals to be present to meet patient needs, being reliable and on-time is critical to keep operations running smoothly. In the post-pandemic world, where many people’s ability to work has been affected, staffing healthcare positions is a constant challenge. Healthcare workers are also trusted to work with expensive equipment, and all supplies must be honestly accounted for and cared for properly. An ethical approach is necessary, embodying principles such as “first, do no harm” and offering just and equitable care for all people regardless of background, income, ethnicity, or sexuality/gender expression.
These values extend to the respect of a patient’s individual rights. Each facility typically provides their own version of these rights, but the general concepts are based on ethical principles, such as autonomy, and include the right to:
- Be treated justly
- Receive accurate information about care
- Refuse treatment
- Confidential medical care
- Continuity of care
- Have pain treated to a level of toleration
- Be free from physical restraints unless the patient is thought to be likely to hurt themself or others
- View their own medical records
- Clear explanations of costs and bills
- Determine and provide advanced directives (Olejarczyk & Young, 2022)
Commitment
Keep in mind that when a healthcare organization hires you, they are investing time and money in your training. By being a part of a healthcare team, you are not only committing your time and energy to your patients but also to your organization and peers. Although every job has some stressful aspects associated with it, coworkers and patients rely on your presence. Gratitude for the opportunity to receive on-the-job training is a positive way to approach a healthcare profession. Be aware that potential employers will evaluate a job candidate’s work history for frequent job changes, which can make it appear as if the candidate lacks commitment. There may be legitimate reasons to change jobs, such as finding a workplace closer to home, but be sure to point out why you left an organization. Resilience and the ability to persevere through difficulties are ways that a healthcare worker might show their commitment. The longer a worker stays in the field the more experience they gain, allowing them to develop professionally and improve their ability to care for patients.
A Story About Commitment From a Healthcare Professional
I first entered healthcare when I worked in the kitchen of a long-term care facility. While I was sweeping after meals in the dining room, the residents would come in and talk to me. They were looking for interaction. I noticed a sign on a bulletin board offering free classes to become a certified nursing assistant. I realized that I could help the people much more if I were in a nursing assistant role, so I signed up for the training. I enjoyed learning about healthcare and my duties. However, when it came to helping people use the restroom and having to change adult briefs for those who could not use the toilet, I hated dealing with feces due to the smell. I thought “this was not what I was expecting when I signed up!” I was ready to quit, but I had started to form relationships and bonds with the residents, so I pushed myself to keep going a bit longer. After a few weeks, I found that the satisfaction of caring for others far outweighed the unpleasant parts of the job, which only lasted a few minutes.
-Anita
Integrity and Trustworthiness
Healthcare professionals are constantly collecting and interacting with patients’ private health and personal information. Keeping that information confidential is a matter of personal integrity as well as a legal requirement. For example, the Health Insurance Portability and Accountability Act, also known as HIPAA, regulates what information can be shared with other healthcare professionals, and what or when information cannot be shared. Training on patient privacy will occur on the job as well as in the educational preparation for the healthcare role. People who are ill, frightened, or relying on the healthcare worker for vital information are in a vulnerable state. The healthcare worker is placed in a position of trust to provide the appropriate care or information and to help people face challenges and solve problems. You will learn more about the laws and ethics surrounding patient information in Chapter 4. In the meantime, understand that regardless of law, healthcare professionals provide better care when they work with integrity.
Communication, Listening, and Emotional Intelligence

Patients have information, concerns, and stories about their lives that help us understand who they are and what is important to them, so healthcare workers need to listen carefully and give people the time to communicate. Along with being able and willing to speak up when something is not right, these critical elements keep others safe in a healthcare environment. In some instances, healthcare professionals may need to provide tools and resources to ensure patients are informed about the healthcare being provided. For example, healthcare professionals in the United States are typically taught how to communicate and write in English. However, for patients and families who do not speak English fluently, interpreters will be used. In this example, healthcare professionals should address the patient directly, and the interpreter will translate.
Healthcare is also a field where different roles must share information about a patient. This is usually done because different healthcare specialists provide different aspects of care, and the information flowing between them must be accurate to prevent errors and potential harm. This extends to healthcare workers being clear with peers or supervisors about their limitations. If a healthcare worker has not been trained on a new piece of equipment or does not know how to do a procedure, they need to be clear about their current understanding so no mistakes are made that could hurt someone. A willingness to slow down and truly, attentively, listen to people can help individuals feel comfortable discussing these kinds of concerns.
Emotional intelligence (EI) is one of the “soft” or “people” skills needed in healthcare workers. One way to describe EI is the ability to understand and manage emotions, which gives healthcare workers insight into interpersonal relationships. EI is not something people are born with. They learn by example and can gain skills that will help enhance relationships (Cavaness et. al., 2020, p. 197). Some examples of emotional intelligence include:
- An ability to identify and describe what people are feeling
- A strong sense of curiosity, particularly about other people
- Feelings of empathy and concern for other people
- Showing sensitivity to the feelings of other people
- Accepting responsibility for mistakes
- The ability to manage emotions in difficult situations
Showing sensitivity to others may be challenging based on a variety of factors, such as a person’s upbringing, cultural expectations, and neurodiversity. Keep this in mind, as it may require increased effort or support to convey recognition of what others are feeling due to your experience and identity, and the level of effort may vary depending on the situation.
Skill Stitch: Applying Emotional Intelligence
Imagine that there is a patient who is angry that they have had to wait 40 minutes for their appointment to start. The person paces up and down the waiting room and keeps sighing and looking at the clock. The healthcare worker uses what they know about EI to recognize and validate what the person is experiencing and acknowledges the concern. “Hello, Ms. Brown, I am sorry it is taking so long. I can see that you are frustrated, and I understand, I would be too. We appreciate your patience. I checked with the team, and you will be the next person to be placed in an exam room. May I offer you a bottle of water while you wait?” This empathetic approach would have more of a positive impact than ignoring the person, and hopefully they would return for care to the same organization in the future.
Time Management and Prioritization
Using work time wisely and keeping up with responsibilities can be challenging in any job. It is especially important when patients and others we serve are counting on the healthcare worker’s ability to multitask. Being able to identify what is most important or urgent and then prioritize your attention is a key aspect of a healthcare job.
A checklist or other notes can help ensure you have remembered each thing that needs attention. Many healthcare workers need to open a patient’s electronic health record to document information, such as blood pressure. Finding time to put information in the record, also known as “charting,” can be problematic, but it is critical for others to be able to see what happened while you worked with the patient, both as a method of communication and a guide to planning the next steps of care.
Job Requirements
All healthcare jobs will list requirements to perform the job. These may include educational preparation, certification or licensure, expectations of prior experience, and physical abilities such as lifting a certain amount of weight or meeting other physical aspects of the job. If you have concerns about specific job requirements for a position you have applied for, you can contact human resources (HR) at your place of work or discuss them in your interview for a position. The U.S. Bureau of Labor Statistics also has in-depth information on job requirements listed alphabetically in their Occupational Outlook Handbook.
Self-Care
Due to the high stress of working with people who rely on them and juggling multiple priorities, healthcare workers need to have a plan for rest and a way to replenish their energy. The demands of the job can deplete a person’s drive and desire to continue their work. For example, healthcare workers can encounter emotionally difficult and traumatic situations, such as someone working with people who have cancer and are suffering or dying. In addition to time and physical/mental/emotional energy, the role may require that the person be on their feet, moving from person to person or place to place for many hours. This alone can cause physical and mental exhaustion. It is okay to ask for help. Reach out to a coworker or your team leader and let them know you are feeling overwhelmed, need assistance to complete specific tasks, or need a short break to reset.
Resources are available for coping, such as spiritual care, employee assistance programs, and mental health counseling referrals. Planning downtime and having methods for managing stress are all critical to preventing burnout and continuing to find fulfillment in your work. Days off with fun activities, getting together with friends, walking in nature, and regular exercise can help reduce stress and occupy the mind with things other than work. Focused and mindful activities such as meditation, artistic hobbies, or prayer can also lower work-related stress. Part of self-care in healthcare is sometimes saying no to extra commitments or extra shifts, especially when trying to schedule time for family and self-care activities. Some healthcare workers may work odd shifts, and when people do not get adequate sleep, they are not able to perform at their best. Lack of sleep not only contributes to building stress but can lead to making mistakes or causing harm. These concerns are why incorporating adequate self-care is a priority within the field today.
During the COVID-19 pandemic, health workers were fearful of getting the virus and had to take on more work than ever. This caused many workers to examine their life priorities, and some of them left healthcare. Those who stayed faced the additional stressor of working without enough staff. Ultimately, each person must decide what is manageable in their life and what is not.
Self-care extends to how healthcare workers protect themselves against certain risks when interacting with patients. Those working in direct patient care need to know how to protect themselves with proper personal protective equipment or (PPE), such as gloves and masks, and get the appropriate vaccinations against viral and bacterial infections, such as COVID-19 and Hepatitis B. These precautions protect patients, but they also ensure that healthcare workers are staying healthy so they can continue to support those patients to the best of their abilities.
Attributions
- Figure 1.2: Clockwise from upper-left: image 1 released under the Pexels License; image 2 released under the Pexels License; image 3 released under the Pixabay License; image 4 released under the Pexels License; image 5 released under the Pexels License; image 6 released under the Pexels License; image 7 released under the Pixabay License.
- Figure 1.3: image released under the Pexels License
- Figure 1.4: PHOTOS INSIDE THE CLASSROOM UPDATED014.jpg by Monirb is released under CC BY-SA 4.0
- Figure 1.5: image released under the Pixabay License
- Figure 1.6: image by Jyothi Gosala is released under Creative Commons Attribution-Share Alike 4.0 International
Clinical laboratories are healthcare facilities that perform a variety of laboratory procedures to help a patient’s care team develop a diagnosis and create a care plan. These laboratories are where blood and other bodily tissues are sent for testing and analysis. A number of health professionals work in clinical laboratories, and in the following sections, we will discuss their roles in greater detail.
Medical Laboratory Technician

Medical laboratory technicians gather collected samples from a variety of bodily fluids and blood. They prepare, process, and test these samples, analyze the results, document and log the data into patients’ medical records, and operate an assortment of lab equipment throughout the process. For example, after receiving a blood sample from a phlebotomist, a medical laboratory technician may perform the required tests, analyze the results, and send the analysis to the care team for evaluation.
Medical laboratory technicians play a critical role in the healthcare team, helping determine a patient’s diagnosis. They are skilled in investigating, identifying clues, and uncovering answers that are vital in guiding patients toward the most appropriate treatment. While their work is often behind the scenes, it is hands-on and essential. For example, technicians may run blood samples through an automatic cell counter or use a microscope to identify pathogens.
Academic Requirements and Career Pathway
The academic requirements for medical laboratory technicians include earning an associate or bachelor’s degree in clinical laboratory science. The training includes both classroom training and hands-on clinical training in the laboratory setting.
After completing the degree program, students are eligible to take the American Society of Clinical Pathology (ASCP) medical laboratory technician certificate exam (American Society of Clinical Pathology, n.d.).
Medical laboratory technicians can pursue specialty certifications in areas such as cytology, hematology, microbiology, molecular biology, blood banking, and chemistry. These credentials allow individuals to specialize in narrower branches of medical laboratory science. For those interested in management or leadership roles within clinical laboratories, advanced degrees are available.
Phlebotomist

A phlebotomist is a healthcare professional who is trained to perform phlebotomy (blood draws) or venipuncture. The blood collected can be used for a variety of tests or donation. A phlebotomist is responsible for preparing patients for the blood draw procedure, which may involve educating them on the process. They ensure that the blood draw site is clean to prevent infection and that blood samples are properly labeled for analysis. They are also responsible for storing and tracking blood samples, which may be sent to other facilities for testing.
Phlebotomists work in various settings, including hospitals, medical offices, blood donation centers, laboratories, skilled nursing facilities, and long-term care facilities.
Academic Requirements and Career Pathway
The academic requirements for a phlebotomist generally include a certificate of completion from a phlebotomy program. Additional education and/or certifications may be required.
Attributions
- Figure 7.8: image released under the Pexels License
- Figure 7.9: image released under the Pexels License
According to the World Health Organization (WHO, 2024), nurses represent nearly 50% of the global healthcare workforce. Nursing is an in-demand career that will always be necessary, making it a stable career to enter. Essential qualities for the nursing role include compassion, patience, communication skills, physical stamina, critical thinking, and good judgment.
In the United States, individuals who are interested in becoming nurses have many options. They can start in entry-level roles such as a nursing assistant, and, if desired, work their way through higher degree programs and certifications to gain additional responsibilities in the healthcare field. There are also multiple terminal doctoral degrees and advanced practice areas in nursing, with many roles in between. This progression is often called the "nursing ladder," as many nurses build on each step of their educational training to move upward in the field. You can also have a fulfilling career without advancing further, especially if you find a specialty that suits you.

The job of a nurse can vary, so this section will focus on the three levels of nursing education: certificate, associate, and bachelor's degrees. We will highlight the differences in scopes of practice between nursing assistants (NAs), licensed practical nurses (LPNs) and registered nurses (RNs).
Certified Nursing Assistants
Certified nursing assistants (CNAs) complete training to provide basic care to patients, assisting with activities of daily living (ADLs). ADLs are activities that we do everyday, such as basic hygiene, eating, ambulation, exercise, getting dressed, using the restroom, and bathing. CNAs may also collect patients’ vital signs. Depending on state requirements, they may also administer medications and perform other duties.
Licensed Practical Nurses
Licensed practical nurses (LPNs), also referred to as licensed vocational nurses (LVNs) in some settings, have a wider scope of practice than CNAs. LPNs/LVNs can monitor patient health, administer care (such as dressing changes, medication administration, and urinary catheter insertions), and report patient status to healthcare providers. They may also reinforce care plans or educational instructions provided by RNs, help collect laboratory samples, and, depending on their training, perform additional tasks such as starting intravenous (IV) medications. LPNs work under the supervision of other healthcare professionals, including RNs, MDs, and NPs.
Registered Nurses
The scope of practice for registered nurses (RNs) is broader than that of other nursing roles. RNs are responsible for physical assessments of patient conditions and may also be responsible for triaging services. In addition to the tasks mentioned above, they develop plans of care for patients and families - this is distinct from prescribing or diagnosing patients - which often includes teaching patients how to manage illnesses or injuries. Additional duties, titles, responsibilities, and skills vary depending on the healthcare setting and any additional certifications or post-RN licensure training.

Employment Opportunities for Nurses
Employment opportunities for nurses are vast. Nurses can work in hospitals, long-term care facilities, clinics, and a variety of other settings, including employee offices, schools, jails, non-profit organizations, and within the community. As mentioned previously, the location and scope of practice for nurses depend on their level of education, training, certification, and licensure.
Employment opportunities abound for nurses at all levels. According to the U.S. Bureau of Labor Statistics (2024), the job growth for nursing careers ranges from 5% for NAs to 6% for LPNs and RNs.
As mentioned previously, education and scope of practice can determine where CNAs, LPNs, and RNs work. In the past, RNs and CNAs were more commonly found in hospitals or acute care settings. However, in recent years, LPNs have become more common in acute care/hospital settings due to staffing shortages. While CNAs are usually less involved in autonomous roles, such as home health or public health, they can work in these areas if the organization can afford to employ them. Long term-care and assisted living facilities commonly employ CNAs and LPNs, although these facilities can employ any level of nurse.
Nurses also have additional opportunities available to them after earning higher-level degrees. Education within the hospital setting or at the college level is an optional path for RNs. RNs may also choose to further their careers by entering hospital administration, conducting research, or exploring roles that measure the quality of hospital care, to name a few.

Requirements and Qualifications
In most states, nursing education, certification, and licensure are highly regulated by the state's department of health and/or nursing commission, as well as by national standards for each educational pathway. Most states require pre-certification or pre-licensure training and examination. Below, we will discuss the requirements for NAs, LPNs, and RNs.
Nursing Assistant Education Requirements and Qualifications
To become a nursing assistant, individuals typically need to complete a course or program lasting 1 to 3 months. Nursing assistant programs include instruction on basic skills, along with a lab and/or clinical work component. These programs can be offered on the job at hospitals and nursing homes, at colleges, and even in high schools.

Depending on the state, there may be additional requirements, such as a state-issued certification, which often includes a competency exam and skills assessment. Individuals are typically referred to as certified nursing assistants (CNAs) or nursing assistants certified (NACs). However, the term "CNA" is commonly used informally to refer to all nursing assistants, even those without certification. Additional certifications may also be available on the job, or with continued training, that allow nurses to acquire more skills, such as medication administration.
Licensed Practical/Vocational Nurse Requirements and Qualifications
To become an LPN/LVN, students must complete an approved educational program, which typically takes about 1 year, although it may take longer with prerequisite coursework. An LPN/LVN, must have a license to practice, and upon completion of their educational program, they should be eligible to sit for the National Council Licensure Examination for Practical Nurses (NCLEX-PN). LPN/LVN programs typically include prerequisite coursework in anatomy, physiology, nutrition, and general education, and the program coursework covers topics such as nursing, patient safety, and pharmacology.
Registered Nurse Requirements and Qualifications
The pathway to licensure as an RN can be through diploma programs (hospital-based training), associate degree programs, and bachelor's degree programs. However, diploma programs have become rare, and many states now require an associate or bachelor's degree in nursing to practice.
An associate degree in nursing (ADN) typically takes 2 years to complete, following 1 year of prerequisites, while the bachelor's degree in nursing (BSN) is a four-year program that includes 2 years of prerequisites, and 2 years of nursing coursework. The biggest distinction between the BSN and ADN programs is that BSN coursework includes a focus on research, public/community health, humanities, leadership and management, health policy and finance, in addition to direct nursing care and clinical judgment. This additional training helps prepare RNs for roles in management, leadership, policy and public/community health.
Whatever the pathway to the RN, students should attend a college or university that is nationally accredited either by the Commission on Collegiate Nursing Education (CCNE), the National League for Nursing Commission for Nursing Accreditation (NLN CNEA) or Accreditation Commission for Education in Nursing (ACEN).
RN programs are typically highly competitive due to the limited number of nursing educators and clinical sites available to meet the demand for both student enrollment and RN job openings in the community. While a 4.0 GPA is not required for admission to an RN program, it can be beneficial. Once admitted, students will complete coursework in nursing concepts, pharmacology, and clinical judgment, as well as skills labs and clinical experiences, usually every quarter or semester.
Once the necessary coursework has been completed, students can sit for the National Council Licensure Exam for Registered Nurses (NCLEX-RN) examination. This is a computer-adaptive exam that needs to be completed at a testing center. Once you pass the NCLEX-RN, you are not required to retake the exam, even if you pursue further education or certification.
Continuing Medical Education
Licensed nurses must meet annual education and practice requirements, which vary slightly by state. In Washington State, both RNs and LPNs must complete eight continuing education hours each year. Practice hours are also required to maintain licensure, which can be earned by working in a clinical environment.
Attributions
- Figure 5.6: image released under the Pexels License
- Figure 5.7: image released under the Pexels License
- Figure 5.8: Collaboration and best in class care: blood cancer by U.S. Department of Veterans Affairs in the Public Domain
- Figure 5.9: image released under the Pexels License
In some small clinics, the same person may handle both the billing and the coding, but medical billing and medical coding are two distinct careers you can train for. Medical coding involves using diagnostic information provided by the physician to assign a particular code for insurance billing purposes. These codes, currently called ICD-10 codes in the U.S., are used internationally (with some countries using the ICD-11 version) to tell the insurance company the patient's specific diagnosis. This allows the company to verify that the corresponding procedural code or office visit code, known as a CPT code, and the related charges are appropriate for the diagnosis. Although medical coding is often integrated into patient chart software, there may still be a need to review codes before submitting them for reimbursement by insurance companies.
Medical coding differs from medical billing in that a medical coder works directly with healthcare professionals but does not always interact with patient records. In contrast, medical billing is done in an office separate from the providers, where patient medical records are frequently viewed.
Here is an example of when a medical biller and a medical coder would be involved in a patient visit:
Sarah hurt her ankle and went to see her primary care doctor. The doctor worked with the medical coder to provide an appropriate diagnosis that would allow insurance to cover imaging and necessary treatment for Sarah's ankle. After the visit, the diagnosis codes and the procedural codes, including those for the office visit and the X-ray, are submitted to the medical biller for processing and submission to Sarah's insurance company. Once the insurance company returns payment, the medical biller will enter the payment information into the system and create a statement to send to Sarah, explaining how much she owes on the balance. If the insurance company denies payment of the claim, the medical coder can review the charge to ensure that it most accurately reflects the patient encounter. Correction and resubmission after a claim denial can lead to a reversal of the original denial, providing payment to the doctor and the clinic for their services. The medical biller can also work with Sarah to establish a payment plan or use charitable forgiveness funds if available.
While medical billing and coding are complementary fields, they may not always be performed by the same person. In the following section, we will discuss the varying options for certification and education in each of these specialties.
Career Opportunities in Medical Billing and Coding
While formal certification or licensure is not required in the field of medical billing and coding, many small practices may have office staff handle medical billing and coding without formal training. However, certification programs in both medical billing and coding can increase your marketability. These programs provide formal exposure to the worlds of medical coding and billing and often include introductory training in medical ethics, HIPPA requirements, and other patient service topics. Many certification programs can be completed in less than a year, making them popular among people looking to re-enter the workforce or change careers.
With a career in medical billing and coding, you can work in a variety of environments. Some people choose to work from home, contracting with different organizations or small clinics that purchase their services. Others may work within a clinical or hospital facility to meet the needs of a single organization. Since medical billing and coding interfaces with third-party payers, career opportunities also exist within insurance companies, where professionals process submitted claims (Bryan University, 2018).
As with many other medical support careers, medical billing and coding specialists are in high demand. For example, some medical coders and billers work specifically with oncologists and cancer treatment organizations to review patient records, pathology reports, and other diagnostic and procedural notes to ensure services are covered by the patient's third-party payer. Other billing specialists, such as those working with anesthesiology practices, ensure the proper coverage and billing of services provided. This may involve coordinating with hospital billing and coding specialists, as some anesthesiologists have private practices that contract with hospitals for their services.
There are different levels of certification for medical coders. These include the certified coding associate (CCA), which requires a high school diploma; the certified coding specialist (CCS), which requires 1 year of experience after obtaining the CCA; and the certified professional coder (CPC), which demonstrates the highest level of expertise in CPT codes and billing. These certifications can be supported by programs at local community colleges and do not require a degree. However, Health IT degrees from two-year or four-year colleges can provide additional training that improves your chances of passing certification exams.
A Day in the Life of a Medical Biller
Gina, 26, starts her day as a medical biller and coder in a neighborhood medical office with 10 providers. She heads to work on the bus, thinking about the projects she is working on in addition to her regular tasks. This month, she has been collaborating with her office manager on a project to increase efficiency and accuracy in their group’s billing performance by reviewing customer feedback.
At work, Gina greets her coworkers and sits down in her cubicle with a cup of tea to get started. She spends the morning processing superbills from her assigned providers’ visits the previous week. A superbill is a form (paper or electronic) that includes the patient’s identifying information, such as their name, date of birth, and patient number, as well as the codes for the patient visit and diagnoses. The visit codes will include a CPT code for the visit itself, any procedures or tests performed, and any modifiers (codes that are required to add procedures and tests to the visit code). Gina double-checks the superbill to ensure that the provider has included all of the correct modifiers. If any modifiers are left out or incorrect, the insurance company will not pay for the additional procedures or tests performed on the day of service.
All of her work is done through a shared electronic medical records (EMR) software, which allows her to view the chart and the patient’s protected health information (PHI) alongside the superbill. She also looks for common errors and compares the visit codes to the diagnosis codes to ensure they align. Finally, she confirms that the insurance information in the patient file matches the information on the superbill and checks for any changes in the file that might affect the claim processing.
After completing her review of each superbill, Gina creates claims using the EMR and sends them electronically to the various insurance companies. For smaller insurance companies, she prints the proper claim form and either faxes it or mails it.
Her morning work done, Gina heads out for lunch and a walk around the block. She makes sure to stretch after spending the morning sitting at her desk.
In the afternoon, Gina processes incoming mail, including insurance payments and payments from patients. She also scans patient payments made through the practice’s online portal, which automatically links payments to patient accounts. She enters any physical payments along with the insurance information about payment adjustments and allowed amounts. Any denied claims are set aside for Gina to follow up on with the insurance companies the following morning.
Since it is the end of the month, Gina also creates billing statements for patients and and prepares them for mailing the next day. At the beginning of the next month, patients whose payments are more than 90 days overdue will receive a phone call from Gina or one of her colleagues before being referred to collections.
Before heading home, Gina reviews the day’s customer feedback surveys and notes a few common issues to discuss with her manager during their weekly meeting. They will brainstorm ways to improve patient satisfaction and retention while ensuring that bills are paid on time. Finally, Gina shuts down her computer, says good night to her coworkers, and heads home, reflecting on all of her hard work as she looks forward to relaxing with a movie.
American Dental Hygienists Association. (n.d.) Professional roles of an RDH. ADHA. https://www.adha.org/education-resources/become-a-dental-hygienist/dental-hygiene-programs/professional-roles-of-an-rdh/
Centers for Disease Control and Prevention. (2018, December 14). Periodontal disease | Oral health conditions. CDC. https://www.cdc.gov/oralhealth/conditions/periodontal-disease.html
Dental Assisting National Board. (n.d.). Washington registered dental assistant requirements. DANB. https://www.danb.org/state-requirements/washington-registered-dental-assistant
Washington State Department of Health. (n.d.) Denturist licensing information. Washington State Department of Health. https://doh.wa.gov/licenses-permits-and-certificates/professions-new-renew-or-update/denturist/licensing-information

Nuclear medicine technologists perform diagnostic exams by administering small doses of radioactive medication to patients. Once the medication is administered, high-tech medical imaging equipment is used to capture images of the radioactive material in the body. In addition to diagnostics, nuclear medicine technologists may also administer radiation internally to treat certain medical conditions.
Nuclear medicine technologists are generally responsible for preparing and administering radioactive medications, recording images to diagnose and treat a patient's condition, and evaluating specimens in the lab.
Nuclear medicine technologists work in hospitals, imaging and medical clinics, diagnostic laboratories, and research centers.
Academic Requirements and Career Pathway
The academic requirements for nuclear medicine technologists include earning an associate or bachelor’s degree in medical imaging with a specialization in nuclear medicine technology (U.S. Bureau of Labor Statistics, 2023). Upon successfully completing their degree program, students can take the Nuclear Medicine Technology Certification Board (NMTCB) exam.
Attributions
- Figure 7.4: Nuclear Medicine Scanner (05810480) by IAEA Imagebank is released under CC BY-NC-ND 2.0
Appropriate Attire
For a job interview, applicants should dress professionally. This includes wearing dress pants or a skirt, a professional shirt, and a sweater or blazer. If the applicant is interviewing for a position in a clinical setting, they may be able to wear scrubs to the interview, or alternatively, they could wear a lab coat over professional attire.
In the healthcare industry, certain items may not be suitable for both the clinical setting and the interview. For example, applicants should be mindful of cosmetics, jewelry, and fragrances. If cosmetics are worn, they should appear natural and understated. Fragrances, including lotions, colognes, and perfumes, should generally be avoided, as many colleagues and patients may be sensitive to scents. Strong smells can cause headaches, nausea, and other health issues. Jewelry should be conservative, and facial piercings should be removed for the interview.
In the clinical setting, nails should be kept short and should not be visible when looking at the palm of the hand. Nails should be clean and well-maintained. Since nail polish, artificial nails, and other nail enhancements are typically not allowed in clinical environments, applicants may want to forgo them during the interview.
Jewelry and accessories should not interfere with clinical duties or patient safety. For example, applicants should opt for smaller earrings or studs rather than large earrings. Hair should be clean and well-groomed, including beards and mustaches. Applicants should refrain from chewing gum during the interview.
Interview Modalities
Many jobs require an interview as part of the application process. Interviews may be conducted in person at a clinical site or office, over the phone, or through online platforms such as Zoom or Microsoft Teams. Some employers also use panel interviews, where multiple interviewers participate in the session.
For online interviews, applicants should ensure they have a stable internet connection and verify the interview link and time in advance. It is recommended to join the meeting early (10 to 15 minutes before the scheduled time) to test the technology and ensure everything is working smoothly. The interview background should be free of distractions, or applicants can use a virtual background or blur the scene. Additionally, applicants should choose a quiet, private space for the interview to avoid interruptions. For example, a noisy café is not ideal; a quiet room in the home with good internet access would be better.
For phone interviews, applicants should also be in a quiet environment with a strong network connection. It is best to avoid outdoor locations with wind, as this can make it difficult to hear. Having a notepad handy is useful for both phone and online interviews, allowing applicants to jot down questions and reflect before answering. Since phone interviews lack nonverbal communication, taking notes will help applicants stay focused. It is perfectly fine to pause before responding or to ask for clarification if a question is unclear.
For in-person interviews, applicants should aim to arrive at least 15 minutes early to allow time for potential delays, such as difficulty finding the interview room. It is advisable to plan the route in advance and check parking arrangements or, if using public transportation, identify the best building entrance. Asking for directions ahead of time is acceptable if needed. Being prepared and arriving early demonstrates punctuality and professionalism.
Behavioral Interviewing
Behavioral Interviewing focuses on asking for examples of past behavior to predict how an applicant will perform in a given role. The idea is that past actions reflect future behaviors, making this type of interview effective in assessing fit for the organization. Although it can be challenging, practicing in advance can help applicants prepare confidently.
One useful method for answering behavioral interview questions is STAR, which stands for:
- Situation: Describe the context or background of the situation.
- Task: Explain the role, job, or responsibility you had in that situation.
- Action: Outline the steps you took to address the situation.
- Result: Share the outcomes or results of your actions.
The STAR method helps structure responses, ensuring they are clear, concise, and focused on key skills relevant to the job.
To further prepare, applicants should review the job description and consider the skills, qualities, and responsibilities the employer is seeking. They should also think of past experiences that highlight these strengths and practice telling those stories using the STAR method. It can also be helpful for applicants to jot down a few notes to bring to the interview, and practice with friends or family beforehand to refine their responses.
Other Interview Styles
Interview questions can vary based on the type of job and employer. In some cases, applicants may be asked to verify credentials. These questions confirm information from the application or ensure the applicant meets minimum job requirements set by the employer's accreditation or regulations. For example, new graduates may be asked if they have passed their certification or licensure exam. Some jobs, such as registered nurse (RN) positions, may conduct interviews before the applicant has passed the exam. In such cases, applicants should be prepared to provide the date of their upcoming exam.
Applicants may also be asked to demonstrate a skill or complete a task during the interview. This is common in fields such as technology, where applicants may need to demonstrate coding abilities or solve a math problem. In healthcare or other service industries, applicants might face case or scenario questions, where they must respond to hypothetical situations, such as how they would handle a particular patient scenario. In these instances, applicants should answer based on their training and how they would approach the situation in a real-world context.
Finally, some applicants may interview with a panel. While this can be intimidating, the principles for responding remain the same.
Follow-Up After the Interview
Although not required, sending a thank-you email after an interview is considered good practice. It is best to send it the same day or as soon as possible afterward. The email does not need to be lengthy but should express gratitude for the interviewer’s time. Additionally, it is a nice touch to mention any enthusiasm you have for the position and to let the interviewer know you are available to provide any further information or answer additional questions.
Non-verbal communication strategies are ways you communicate without speaking, for example through facial expressions, hand gestures, eye contact, and body language. See Figure 2.5.

Figure 2.5: Non-verbal communication
In many situations, much of your communication occurs through non-verbal behaviours. Non-verbal communication can be a useful strategy for communicating emotions like empathy, compassion, and acceptance. It is often how nurses respond, rather than what they say, that leaves a lasting impression on clients, so it is important to be aware of how you communicate using non-verbal behaviours.
Non-verbal behaviours must align with your verbal behaviours so that clients clearly understand what you are saying. For example, it would be confusing for the client if you had a somber tone of voice, distancing posture, and avoided eye contact while attempting to maintain a therapeutic relationship with the client.
Try to ensure positioning where you are both at the same vertical level and a slight angle towards one another. This positioning conveys an open and non-confrontational and non-authoritative space. Whenever possible, avoid standing over the client if they are sitting or lying in bed. It is better to sit down, which also conveys that you have time to listen to them.
There are many models to inform your non-verbal communication. One helpful model is called SURETY (Stickley, 2011) reflected as a modified version in Figure 2.6:
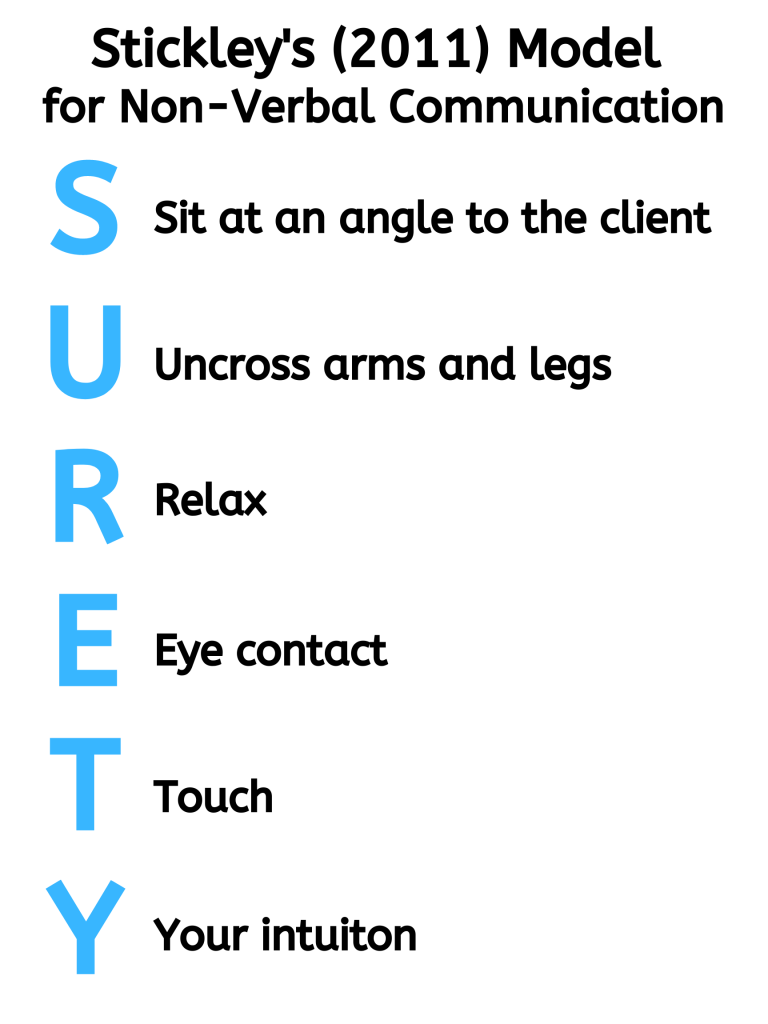
Figure 2.6: The SURETY model.
Points of Consideration
Physical touch
Touch can be therapeutic with clients when used appropriately. It can convey empathy and compassion. You should strike a balance about when it is therapeutically appropriate and when it is an intrusion for clients. It will take practice to learn when touch is appropriate.
Activity: Check Your Understanding
The original version of this chapter contained H5P content. You may want to remove or replace this element.
Acute and Chronic Diseases
The duration of the period of illness can vary greatly, depending on the pathogen, effectiveness of the immune response in the host, and any medical treatment received. For an acute disease, pathologic changes occur over a relatively short time (e.g., hours, days, or a few weeks) and involve a rapid onset of disease conditions. For example, influenza (caused by Influenzavirus) is considered an acute disease because the incubation period is approximately 1–2 days. Infected individuals can spread influenza to others for approximately 5 days after becoming ill. After approximately 1 week, individuals enter the period of decline.
For a chronic disease, pathologic changes can occur over longer time spans (e.g., months, years, or a lifetime). For example, chronic gastritis (inflammation of the lining of the stomach) is caused by the gram-negative bacterium Helicobacter pylori. H. pylori is able to colonize the stomach and persist in its highly acidic environment by producing the enzyme urease, which modifies the local acidity, allowing the bacteria to survive indefinitely.2 Consequently, H. pylori infections can recur indefinitely unless the infection is cleared using antibiotics.3 Hepatitis B virus can cause a chronic infection in some patients who do not eliminate the virus after the acute illness. A chronic infection with hepatitis B virus is characterized by the continued production of infectious virus for 6 months or longer after the acute infection, as measured by the presence of viral antigen in blood samples.
In latent diseases, as opposed to chronic infections, the causal pathogen goes dormant for extended periods of time with no active replication. Examples of diseases that go into a latent state after the acute infection include herpes (herpes simplex viruses [HSV-1 and HSV-2]), chickenpox (varicella-zoster virus [VZV]), and mononucleosis (Epstein-Barr virus [EBV]). HSV-1, HSV-2, and VZV evade the host immune system by residing in a latent form within cells of the nervous system for long periods of time, but they can reactivate to become active infections during times of stress and immunosuppression. For example, an initial infection by VZV may result in a case of childhood chickenpox, followed by a long period of latency. The virus may reactivate decades later, causing episodes of shingles in adulthood. EBV goes into latency in B cells of the immune system and possibly epithelial cells; it can reactivate years later to produce B-cell lymphoma.
Footnotes
- 1F. Savino et al. “Pain Assessment in Children Undergoing Venipuncture: The Wong–Baker Faces Scale Versus Skin Conductance Fluctuations.” PeerJ 1 (2013):e37; https://peerj.com/articles/37/
- 2J.G. Kusters et al. Pathogenesis of Helicobacter pylori Infection. Clinical Microbiology Reviews 19 no. 3 (2006):449–490.
- 3N.R. Salama et al. “Life in the Human Stomach: Persistence Strategies of the Bacterial Pathogen Helicobacter pylori.” Nature Reviews Microbiology 11 (2013):385–399.
Respiratory care is an area of healthcare that specializes in the promotion of optimal cardiopulmonary function, health, wellness, and treatment. In this section, we will discuss respiratory therapy.
Respiratory therapists (RTs) work with individuals of all ages who have trouble breathing. They are typically found in hospitals, rehabilitation centers, nursing homes, emergency rooms, and even on medical flight teams.
RTs assess patients with respiratory issues in both routine and emergency care settings. They evaluate lung function, oxygen levels, and other respiratory parameters to determine the underlying problem. They also conduct diagnostic testing, such as pulmonary function tests and sleep studies. Based on these assessments and diagnostic test results, an RT develops a personalized treatment plan for the patient. Once the treatment plan is implemented, the RT may administer a variety of therapeutic interventions, including oxygen and medication therapies.
Patient education is an important aspect of an RT’s role. For example, in a cardiopulmonary rehabilitation unit, chronic obstructive pulmonary disease (COPD) patients may need instruction on the proper use of bronchodilator medications and sputum clearance techniques.
If you are interested in being a lung expert, working closely with patients, and learning about respiratory diseases, this could be a good fit for you!
Employment Opportunities for Respiratory Therapists
Employment opportunities for respiratory therapists are promising. The U.S. Bureau of Labor Statistics (2024) projects a 14% growth in employment from 2021 to 2031, which is much faster than the average for all occupations. With the growing population of older adults in the United States, there will be an increasing demand for respiratory therapists to address the higher prevalence of pneumonia, COPD, and other changes in lung function due to age or disease.
Areas affected by wildfire smoke, air pollution, frequent use of wood stoves and fireplaces, or communities with high smoking rates are likely to see increased demand for respiratory therapists. In Washington State, for example, increasing smoke from wildfires is expected to increase the need for RTs in the foreseeable future.
About 82% of respiratory therapists work in hospitals, 4% in long-term care facilities, and 2% in physician offices, according to the U.S. Bureau of Labor Statistics (2024). As mentioned previously, in hospitals or acute care settings, RTs may work in intensive care units or emergency rooms. They may also work in patients' homes, sleep laboratories, case management programs, asthma education programs, smoking cessation programs, air transport, ambulance services, and physicians’ offices.

Respiratory Therapy Requirements and Qualifications
An associate degree is typically required to become a respiratory therapist, although there is a growing demand for bachelor's degree programs, especially in urban areas. Most respiratory therapy programs have limited admission and require prerequisite coursework in general education subjects such as anatomy and physiology, psychology, English, and math. Once accepted, students will study pharmacology, respiratory care sciences, and management across the lifespan, and will complete clinical coursework.
In the United States, the Commission on Accreditation for Respiratory Care (CoARC) is the accrediting body for respiratory therapy programs. CoARC uses an outcomes-based process to document program effectiveness. Accreditation information can be found on the website of any accredited respiratory care program.
After completing an associate or bachelor's degree, students are eligible to sit for the Therapist Multiple-Choice Examination (TMC), which evaluates the abilities required for entry into respiratory therapy practice. The certified respiratory therapist (CRT) credential is awarded to those who pass the TMC examination. Upon passing the TMC, candidates are eligible for the Clinical Simulation Examination (CSE). The CSE must be passed to earn the registered respiratory therapist (RRT) credential, which is considered the standard of excellence, according to the National Board for Respiratory Care. RRTs can also take sub-specialty examinations in areas such as adult critical care, neonatology/pediatrics, or sleep disorders.
Attributions
- Figure 5.13: Respiratory therapist at Baystate Health NICU.jpg by Rose State Community College. is released under Creative Commons Attribution 2.5 Generic license.

