2.2 The U.S. Healthcare System
Anita Hedlund

Healthcare in the United States is complex. The United States has the third-largest population in the world after China and India (approximately 335 million people), yet it has the world’s highest healthcare expenditure. Rather than a nationalized healthcare system, in the United States, “there are multiple insurers and delivery systems that are often uncoordinated” (Rice et al., 2020, p. 29).
Most patients in the United States are either paying out-of-pocket for healthcare services or paying private healthcare insurance to assist in covering costs. Because of this model, and the high cost of healthcare, lack of insurance coverage is a major barrier to public health. About 10% of the U.S. population has no health insurance, not necessarily because of unemployment but because the cost of coverage is too high (Tolbert et al., 2022). Additionally, the Commonwealth Fund (2022) found that 43% of working adults were underinsured in 2022, meaning that they had some insurance but it was insufficient for their healthcare needs. This contrasts with countries such as the United Kingdom, Germany, Switzerland, France, and Singapore that use socialized medicine. Socialized medicine is a healthcare system in which medical and hospital care is funded by public resources, primarily through taxes. In socialized medicine, all healthcare, including the employment of healthcare workers, is run by the country’s government.
Rice et al. (2020) state that strengths of the U.S. healthcare system are a “large and well-trained health workforce and a wide range of high-quality medical specialists, as well as secondary and tertiary institutions, a robust health sector research program and . . . among the best medical outcomes in the world” (p. 333). However, it should be noted that even though some U.S. medical outcomes, such as the survival rate of certain cancers, are among the best in the world, other conditions, such as asthma, may have poorer outcomes. There is also inconsistency in managing health behaviors through public messaging, with the United States being “notably effective in reducing smoking rates but equally ineffective in grappling with nutritional health and obesity” (Rice et al., 2020, p. xxiii).
Sadly, although the United States has a well-educated workforce and high-tech equipment, its mortality rate is worse than that of other countries with similar offerings. The Population Health Forum (2019) points out that the United States is the richest yet sickest nation in the world, with the largest gap in health outcomes between the wealthy and the poor. As the healthcare system grapples with these gaps, healthcare professions will need to consider how to address health equity or, in other words, provide the necessary support to ensure all people can attain their highest level of health regardless of identity or background.
The Centers for Disease Control and Prevention (CDC, 2022b) have indicated that key lifestyle choices are major contributors to U.S. health problems. The use of tobacco, poor nutrition (such as too much deep-fried food with not enough nutrients), lack of physical activity, and excessive alcohol consumption contribute to six out of ten Americans having some type of chronic disease such as heart disease, respiratory diseases, diabetes, and substance abuse. Compared to other industrialized nations, the United States is 36th in the world when it comes to life expectancy, and the infant mortality rate is two to three times that of most other developed nations.
Lack of equitable access is another concern in the United States. Not all people have the same opportunities to access healthcare. Access can be affected by disabilities, distance to healthcare facilities, lack of transportation, cost of fuel, lack of childcare, and racial or gender inequalities. Consider a common barrier to equitable access: lacking health insurance. It is no surprise that the majority of uninsured people are in low-income families, with the cost of insurance being too high, even when at least one member of the family works (Tolbert et al., 2022). Depending on the state, there may be limited availability of coverage that disproportionately affects adults, the elderly, and those who identify as people of color (Tolbert et. al., 2022). Sadly, many people avoid needed healthcare or medication due to cost, even to the point where they experience immense impacts to their health and daily life. Even for the insured, some medications cost several hundred dollars a month for one prescription, again disproportionately affecting those with limited income.
Disease Dissection: Diabetes
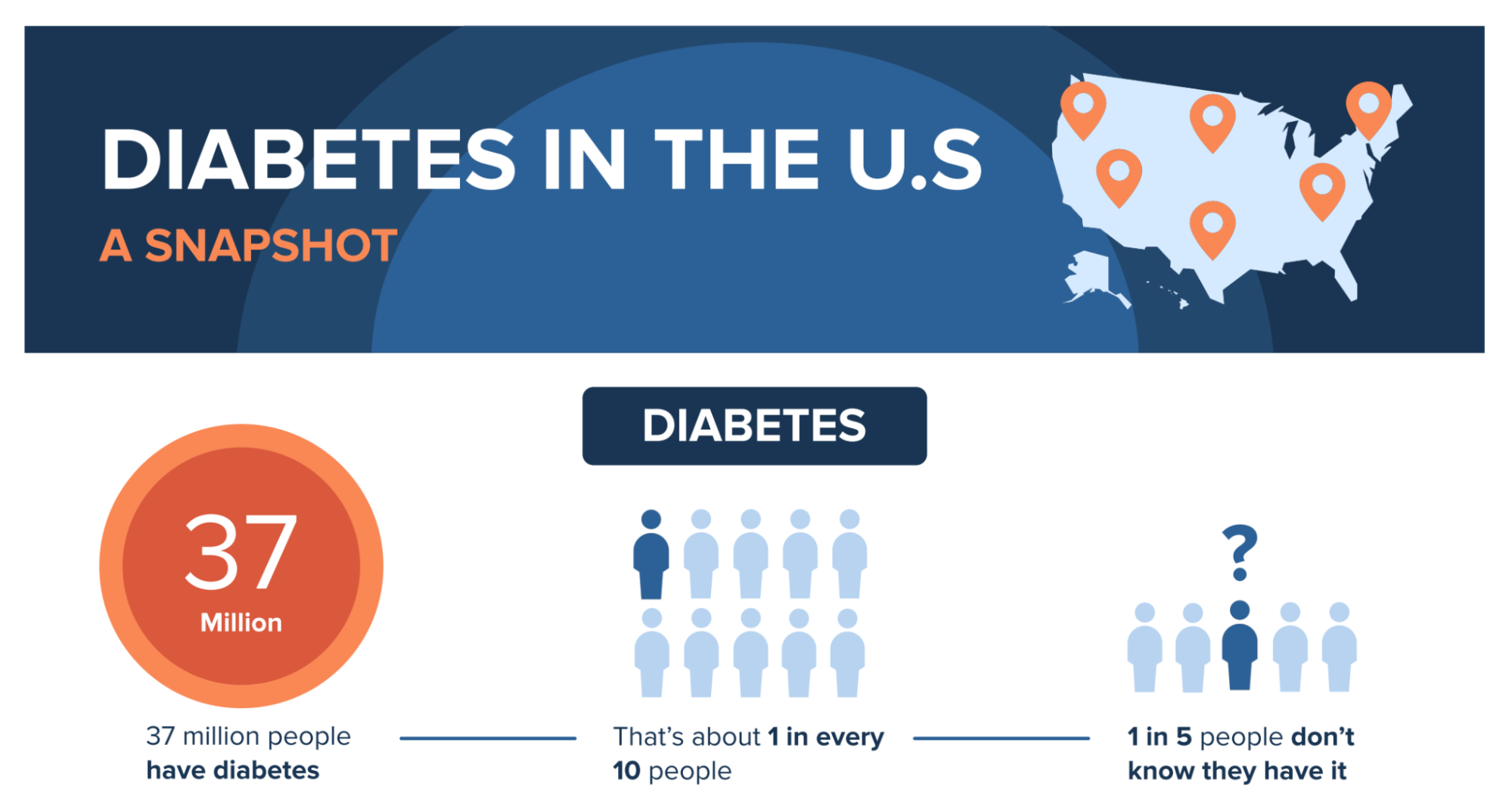
If you work in healthcare, you will no doubt encounter people with diabetes. There are several types of diabetes, but this section will cover the most common form, diabetes mellitus (DM). DM has to do with the body’s regulation of sugar, in the form of glucose. Human bodies need glucose to provide energy to the cells that make up the muscles and tissues, and it is the main fuel source for the brain. In order to have the right amount of glucose available in the bloodstream, the body has to produce enough insulin. Insulin is like a ferry that transports glucose into certain cells. If the body does not produce enough insulin to carry all the glucose into the cells, the excess accumulates in the blood and is then processed by the kidneys and excreted in urine. This accumulation of glucose in the blood leads to the numerous symptoms and complications that result from this chronic disease.
Complications from diabetes, primarily heart and kidney disease, are extremely impactful to U.S. healthcare. The total estimated cost of diagnosed diabetes in 2017 was $327 billion, including $237 billion in direct medical costs and $90 billion in lost productivity. Cardiovascular disease (CVD), a condition in which the heart and blood vessels are negatively impacted by a variety of factors such as high cholesterol and high blood pressure, is the number one cause of death for people living with diabetes. Fortunately, these risks can be decreased with medications, proper diet, and exercise.
If you want to learn more about diabetes, the American Diabetes Association and the Centers for Disease Control’s Basics of Diabetes and Diabetes by the Numbers are great places to start.
How Health Costs Are Paid For
The importance of health insurance to the U.S. healthcare system cannot be overstated. It provides important financial protection in case you have a serious accident or sickness. As discussed above, people without health coverage are exposed to high costs that can sometimes lead them into deep debt or even bankruptcy.
It is easy to underestimate how much medical care can cost. For example:
- Fixing a broken leg can cost up to $7,500.
- The average cost of a three-day hospital stay is around $30,000.
- Comprehensive cancer care can cost hundreds of thousands of dollars. (Tolbert et. al., 2022)
Having health coverage can help protect you from high, unexpected costs such as these.
Options for health insurance in the United States include one of the many private insurers or, if a person qualifies, one of the two government programs for the general public, Medicare and Medicaid.
Medicare
Medicare is health coverage for people who are over the age of 65, with some exceptions for qualifying conditions. Navigating Medicare is complex, as it has multiple parts: A, B, and D. According to the Centers for Medicare & Medicaid Services (2024a), “Medicare covers most, but not all of the costs for approved healthcare services and supplies. After you meet your deductible, you pay your share of costs for services and supplies as you get them. There’s no limit on what you’ll pay out-of-pocket in a year unless you have other coverage.” If you go to a doctor or other healthcare provider that accepts the Medicare-approved amount, your share of costs may be less. If you receive a service that Medicare does not cover, you pay the full cost.
For Medicare to cover a healthcare service, it must be justified as medically necessary. However, Medicare will cover some preventive services, such as shots and screenings. Services such as long-term care or cosmetic procedures are not included in standard Medicare coverage.
Medicaid
The other federal healthcare program, in partnership with state governments, is Medicaid. “Medicaid provides health coverage to millions of Americans, including eligible low-income adults, children, pregnant women, elderly adults and people with disabilities. Medicaid is administered by states, according to federal requirements” (Centers for Medicare & Medicaid Services, 2024b).
The Children’s Health Insurance Program (CHIP) was signed into law in 1997 and provides federal matching funds for states to provide health coverage to children in families with incomes too high to qualify for Medicaid but who cannot afford private coverage.
Through the Basic Health Program, states can provide coverage to individuals who are citizens or lawfully present non-citizens who do not qualify for Medicaid, CHIP, or other minimum essential coverage and have income between 133% and 200% of the federal poverty level (FPL). According to the U.S. Department of Health and Human Services (2023), in 2023, the FPL for a family of four was $30,000.
Private Insurance
Private insurers often contract with an employer/organization to provide health insurance to employees, which means that coverage for the vast majority of the insured is tied to employment. Typically, the employer pays most of the monthly fee as part of a benefits package. However, a percentage of the cost must be covered by the employee. For those who are self-employed, or employed without access to employee benefits, insurance coverage can be purchased directly.
U.S. Health Policy
The U.S. healthcare system cannot be discussed without acknowledging the role of politics in health policy. Health policy can be an important platform for political parties running for office, and health policy changes depending on which political party is in power, subject to the election cycle every 2 to 4 years.
Politics plays an important role in health policy because the power to enact health policy, such as regulation of pharmaceuticals and medical devices, resides partially in the federal government. However, individual states “fund and manage many public health functions, pay part of the cost of Medicaid and shape its organization within that state, and set the rules for health insurance policies that are not covered by self insured employer plans” (Rice et al., 2020, p. xxiv). This balance of power between federal and state governments allows for states to determine elements of health policy based on their own constituents, but it also results in major variations in policy from state to state.
The federal agency that oversees healthcare is the Department of Health and Human Services, which in turn oversees the Medicare and Medicaid programs through its Centers for Medicare and Medicaid Services (CMS). Other health-related federal agencies include the National Institutes of Health, the Centers for Disease Control and Prevention, the Veterans Health Administration, and the Food and Drug Administration, and each plays an important part in shaping U.S. health policy.
A Look at the Veterans Health Administration
The Veterans Health Administration is a federal agency set up to take care of people serving in or retired from the military and their families. It runs a network of hospitals and clinics throughout the country. However, these military facilities can only be used by select patients with disabilities and the highest care needs. Care is given to those who need it the most.
Once military personnel separate from service, they are offered an option to take TriCare insurance or private insurance. They can also choose to be seen either at military facilities or the same hospitals that are available to everyone.
Evaluating Healthcare
The reliance on public funds or private insurance to cover most healthcare costs creates many jobs in planning and evaluating the care provided (utilization review or case management), assigning codes (medical coder), and billing (billing specialist). Current Procedural Terminology (CPT) codes are used to track and bill medical, surgical, and diagnostic services performed. These must be used in order to get reimbursement by insurance companies (American Academy of Professional Coders [AAPC], 2023). Hospitals and providers are reimbursed by insurance on a fee-for-service basis. To improve outcomes and quality of healthcare, Medicare will no longer reimburse for certain preventable problems such as hospital-acquired infections.
The Center for Medicare Services (CMS) and other national organizations such as the Joint Commission survey healthcare facilities and audit medical records to assess the quality of care being provided. These audits involve determining whether services provided to patients were appropriate, and what, if any, medical errors were made. The surveyors ensure that state and federal laws, as well as the institution’s own policies, are being followed. These audits may also evaluate the physical environment in which care is provided, looking at everything from sanitation practices to fire safety. This is done to protect the public and to guarantee that patients are receiving the best and safest medical care.
Attributions
- Figure 1.7: image released under the Pixabay License
- Figure 1.8: image by CDC in the Public Domain
- Figure 1.9: Maryland National Guard by The National Guard is released under CC BY 2.0 DEED
Welcome to Introduction to Allied Health, compiled by Rebekah Ramsey and April Bruns of the College of Southern Idaho! As you can see from our attribution section, we have gathered together chapters from three other OER books and multiple articles related to allied health, technology, COVID, and other matters to create a digital textbook that should most thoroughly fit the needs of the students at CSI. This is, of course, a work in progress, but we put time and effort beforehand into finding, ordering, arranging, and integrating these chapters. Keep in mind that some chapters may specifically mention nursing only, but the content is relatable for many allied health careers. There may also be more detailed information and examples used from specific states (such as Washington healthcare law). Please let us know if you have any issues trying to access the chapters, or if you have any questions regarding the content.
Introduction
Early in the year 2020, the rapid spread of COVID-19 brought nearly everything in the world to a screeching halt. From schools closing to economies crashing to permanent lockdowns, it has seemed as though every aspect of life has been affected. With few exceptions, these effects have had a negative connotation to them. People have lost their jobs, social interaction has been limited, and hundreds of thousands or people have lost their lives. Unfortunately, months later and the pandemic is still raging as strong as ever. However, obstacles and crises, especially ones on the scale of the Coronavirus pandemic often create permanent change to the way society functions. COVID-19 has undoubtedly revealed many flaws in and created many obstacles for today’s society. However, its impact has reshaped the world of healthcare and will promote advances in medicine long into the foreseeable future. These advances include the implementation of tele-health services, big data analysis, development of new medical manufacturing, and fixing racial disparities in healthcare.
Connection to STS Theory
COVID-19's impact on the medical community relates directly to the Path Dependency theory. Path Dependency, in the study of science, technology and society argues that decisions people make in the present are influenced by events that have occurred in the past. Developments in human society, according to Path-Dependency are shaped by a sequence of past events. Past events shape the present and future by limiting the options and choices available to people when they make decisions. Coronavirus has caused nearly everything in daily life to be changed. Precautions must be considered when doing anything that used to be so simple. Although some of these changes may seem like a nuisance now, they are going to make life in the future much simpler by advancing new technological innovations. Due to COVID-19, important health advice will be available at the touch of people’s fingertips, robots will provide smoother and quicker healthcare operations, and technology such as 3D printing will help prevent medical supply shortages. Future outcomes are altered by what is happening in the present. While the most unfortunate way to learn from the past is for people to lose their lives, this loss will also have the greatest impact on the push for change.
Another idea with a strong connection to healthcare and COVID-19 is modernization. This seems contradictory considering failings of the many healthcare systems, particularly in the United States in dealing with the Coronavirus. Some may argue that Coronavirus has resulted in almost the opposite of modernization, causing healthcare to regress rather than progress. They point out that COVID-19 testing hasn’t been smooth, there have been many inconsistencies in information about the virus, and there have been many shortages of ventilators and room in hospitals. More importantly, spread of the virus was poorly contained and hundreds of thousands of people have lost their lives because of this. Although these are truly unfortunate developments, they do not outweigh the overall modernization of health care throughout the pandemic. Innovation to tele-health services and other inventions have helped to overcome some of problems created by COVID-19. New innovations, more importantly, will change the future of medicine and health services, creating more adequate care for society.
Issues that Coronavirus has Exposed
As of the date November 29th, 2020 almost 13.3 million United States citizens have been infected with COVID-19 and roughly 266,000 people have lost their lives (The New York Times). The United States, along with the rest of the world, was obviously not prepared for a pandemic - especially a one of this magnitude and severity. Throughout the pandemic, numerous shortages of necessities for containing the spread of COVID-19 caused even more problems. During lockdowns stores seemed as though they had been looted. Aisles upon aisles of completely empty shelves made it impossible for customers to acquire essential products such as toilet paper, masks, and cleaning supplies. On the homefront many people were forced into working from their homes and students explored attending school online.
Although many parts of society were unprepared, COVID-19 truly exposed the flaws and unpreparedness within the medical community. As a result of previous unpreparedness, hospitals quickly became overwhelmed by an influx of patients and didn’t have beds for everyone. While the number of patients were increasing, the number of medical personnel available were decreasing as they were infected. Additionally, one of the most common symptoms of Coronavirus is shortness of breath and difficulty breathing. COVID-19 patients often need to be put on ventilators to help them breath. However, patients in intensive care units were struggling more than they should due to the lack of available ventilators. In other cases, there was just no way to get patients a ventilator.
Despite all these issues, the one that seemed most problematic was the inability to get tested. Towards the beginning of the pandemic, testing times would sometimes need to be determined weeks in advance. Without officially testing positive for the virus it seemed difficult to force someone into quarantine for ten to fourteen days. While there have been improvements, it still can take a significant amount of time to receive the results of the test. In some cases, this waiting time could be up to five days. If the results were to come back positive, there is a good chance that the person would have exposed a lot of other people. The lack of capacity to efficiently test and provide quick results has undoubtedly been one of the biggest contributing factors to why COVID-19 is spreading so quickly.
Advances in Telehealth Services

As a direct result of the Coronavirus, the medical world has already seen significant improvements and will continue to see innovations long into the foreseeable future. One area that jumps out as having the most potential for better healthcare post COVID-19 is telemedicine. To give some background, telemedicine is the distribution of health-related services and information through telecommunication technologies. In other words, it provides virtually the possibility of long-distance patient care, advice, and monitoring. Telehealth was around prior to COVID-19, it has just seen an increase in use during the pandemic. Over the years not everyone has been fully supportive of employing telemedicine. In fact, back in 2014 the Texas Medical Society even went as far as to vote it illegal (Shaywitz). The arguments in opposition to tele-health have stemmed both from patients and the doctors. Doctors worry that their patients won’t actually use the service and that they will not be compensated for it because the service is online. On the other hand, patients feared that online services will be too complicated and not as adequate as going in person to the doctor.
However, just as all aspects of life have experienced a serious change from COVID-19, so has tele-health. As hospitals quickly reached capacity at the beginning of the pandemic, it became extremely important to keep medical personnel healthy. The obvious yet difficult way to accomplish this was to decrease contact between highly contagious patients and the doctors. As a result, tele-health prevailed as the most efficient way to decrease this contact. Despite the concerns of both patients and doctors, research has been done to prove that tele-health is in fact a sufficient replacement and will continue to be in the post pandemic era. A study conducted by 11 mental healthcare professionals in April 2020 concluded that mental healthcare will consist of a blended format of online and in person treatment in the future (Bierbooms et al.). Despite a limited use of the approach, the tremendous success of tele-health during the initial phases of the pandemic has yielded hope that its future potential is unlimited. Over the years, health care providers have been slowly attempting to make more services available via tele-health. Although progress has been slow, leaders across the ideological spectrum agree that COVID-19 has pushed the inevitable tele-health revolution forward by more than a decade. (Facher). This rapid improvement will ensure the success of tele-health in the future of healthcare.
Medical Inventions from COVID-19

While the Coronavirus had led to innovation, as seen in the case of tele-health, it has also directly produced inventions. Hospital intensive units in the early pandemic were rapidly filling with people in need of ventilators. Unfortunately, the supply of ventilators was not meeting the demand. In response, developers at Army Research Laboratory collaborated with civilian partners to create low-cost, 3D printed ventilators to help struggling patients stay out of the ICU. Additionally, they used this same printing process to create other necessities such as masks (Brading). The significance of these inventions is to demonstrate the potential for 3D printed medical devices. The ease of use, in addition to the low cost of 3D printing is revolutionizing product development. Manufacturers of medical tools have been adopting this technology to produce brand new medical devices and surgical instruments. Regular citizens who have 3D printers at home can also help to alleviate the medical supply shortage by printing out masks.
Another groundbreaking development was a robot that Johns Hopkins University designed to operate ventilators remotely, without humans having to be inside the room (Robots). With the shortage of protection, mainly masks and gloves for medical personnel becoming a problem it was unreasonable to continue switching protective gear and disinfecting patients' rooms every time a ventilator needs to be adjusted. The Johns Hopkins robot overcame this issue because doctors won’t physically have to be in the room with the patient. Similar to tele-health services, this is so important because it protects hospital staff from highly contagious patients. However, this robot will be useful even after the Coronavirus pandemic. In addition to providing protection to doctors, its ability to allow many patients to be treated simultaneously and quickly is essential for the future. As seen in this pandemic when hospitals fill up, there must be a way to treat all patients.
Bid Data and Disparities in Medicine
Trying to target hotspots of the Coronavirus and contact tracing have proven to be extremely difficult throughout the pandemic. While some of the problem is people refusing to follow restrictions, being able to understand numbers and data quicker could significantly reduce the spread of the virus. Medicine and health in general have long awaited this revolutionary change in terms of big data. This would mean massive amounts of data coming straight from patients and populations, with advanced analytics to give it meaning. In a recent study it was determined that in a group of 142 FM physicians, doctors spent on average nearly 6 of their 11-hour days working on Electronic Health Records (EHRs) (Hughes). Transforming the way this data is handled and analyzed would significantly improve the efficiency of doctors by giving them more time to actually treat patients. Furthermore, the potential for big data in medicine could provide major improvements in areas such as reducing costs, understanding population health trends, and patient outcomes. The inability to successfully analyze big data sets related to the Coronavirus has clearly demonstrated how badly this change needs to be implemented.
Finally, for years a deeply rooted problem in society has been the racial and ethical disparities in health care. While this issue has been severely overlooked, Coronavirus data is helping to bring the problem back into the spotlight. For example, African Americans represent a small 6 percent of Wisconsin’s population (Wisconsin Department of Health Services). Somehow however, the minority accounts for almost half of the coronavirus related deaths in many parts of the state (Hess). Unfortunately, this is not an isolated case. Across the country numbers are showing that COVID-19 is killing people of color at staggeringly disproportionate rates. This can be directly related to a person's socioeconomic position impacting the level of health care they receive. Based on the theory of path dependence, there is some hope that these numbers will prompt long overdue changes needed to fix the racial disparities in health care.
Conclusion
These developments are merely a glimpse at the revolution in medical technology that COVID-19 has spurred. Hopefully, this modernization and improvement will prevent a future pandemic from tearing apart society as COVID-19 did. With that being said, the repercussions that Coronavirus caused cannot be completely overlooked. Hundreds of thousands of people have lost their lives and COVID-19 cases have continued to skyrocket. Almost every aspect of normal life has been altered in some form by the virus. These negatives outcomes, however, have invoked change in society. In the medical community the main changes are in improving patient outcomes, doctor's efficiency, and keeping medical personnel safe. These reforms are not solely isolated to the medical sector. In fact, many other areas of life are seeing similar advances as they adapt to new norms after suffering initial setbacks. This process clearly highlights the theory of path dependence in studies of science, technology and society. Even prior to the pandemic, society has shifted its gears to produce technology that will help solve problems it faces. In the pandemic technology has been used address problems caused by Coronavirus and to make sure that mistakes of the past are not repeated in the future. As a result, despite the some of the unfortunate outcomes, COVID-19 has ultimately advanced medicine and made life better off in the future.
References
Bierbooms, Joyce, et al.“Integration of Online Treatment Into the ‘New Normal’ in Mental Health Care in Post–COVID-19 Times: Exploratory Qualitative Study.” JMIR Preprints. preprints.jmir.org/preprint/21344/accepted.
Brading, Thomas. “Army Researchers Help Design 3D-Printed Ventilators.” US Army, 1 May 2020, www.army.mil/article/234822/army_researchers_help_design_3d_printed_ventilators.
Facher, Lev, et al. “9 Ways Covid-19 May Forever Upend the U.S. Health Care Industry.” STAT, 19 May 2020, www.statnews.com/2020/05/19/9-ways-covid-19-forever-upend-health-care/.
Hess, Corrinne. "3 Times More Likely To Die': Coronavirus Ravages Milwaukee's African American Community." Wisconsin Public Radio, 12 May 2020, https://www.wpr.org/3-times-more-likely-die-coronavirus-ravages-milwaukees-african-american-community.
Hughes, Jonathan Ford. “How Will Medicine Look in the Future?” Physician Sense, 29 May 2020, www.mdlinx.com/physiciansense/how-will-medicine-look-in-the-future/.
“Robots Joining the Front Lines to Battle COVID-19.” YouTube, uploaded by Johns Hopkins Medicine, 14 Aug. 2020, www.youtube.com/watch?v=ZG6RdPfghJs&feature=youtu.be.
Shaywitz, David. “How Will Coronavirus Change the Health-Care Industry?” National Review, 1 Apr. 2020, www.nationalreview.com/2020/04/coronavirus-pandemic-health-care-permanent-changes/.
The New York Times. “Covid in the U.S.: Latest Map and Case Count.” The New York Times, 3 Mar. 2020, www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html.
Wisconsin Department of Health Services. "COVID-19: Racial and Ethnic Disparities." Wisconsin Department of Health Services, https://www.dhs.wisconsin.gov/covid-19/disparities.htm.
Images
"Telemedicine Consult" by Agathe Padovani is licensed under CC BY-SA 2.0
"Q-vent" by TomCatOne is licensed under CC BY-SA 4.0

