Perspectives on Abnormal Behavior
2.3 The Biological Model
Alexis Bridley & Lee W. Daffin Jr. and Carrie Cuttler
Section Learning Objectives
- Describe how communication in the nervous system occurs.
- List the parts of the nervous system.
- Describe the structure of the neuron and all key parts.
- Outline how neural transmission occurs.
- Identify and define important neurotransmitters.
- List the major structures of the brain.
- Clarify how specific areas of the brain are involved in mental illness.
- Describe the role of genes in mental illness.
- Describe the role of hormonal imbalances in mental illness.
- Describe commonly used treatments for mental illness.
- Evaluate the usefulness of the biological model.
Proponents of the biological model view mental illness as being a result of a malfunction in the body to include issues with brain anatomy or chemistry. As such, we will need to establish a foundation for how communication in the nervous system occurs, what the parts of the nervous system are, what a neuron is and its structure, how neural transmission occurs, and what the parts of the brain are. While doing this, we will identify areas of concern for psychologists focused on the treatment of mental disorders.
Brain Structure and Chemistry
Communication in the Nervous System
To really understand brain structure and chemistry, it is a good idea to understand how communication occurs within the nervous system. Simply:
- Receptor cells in each of the five sensory systems detect energy.
- This information is passed to the nervous system due to the process of transduction and through sensory or afferent neurons, which are part of the peripheral nervous system.
- The information is received by brain structures (central nervous system) and perception occurs.
- Once the information has been interpreted, commands are sent out, telling the body how to respond, also via the peripheral nervous system.
Please note that we will not cover this process in full, but just the parts relevant to our topic of psychopathology.
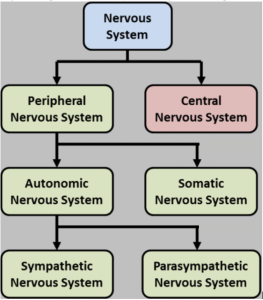
The Nervous System
The nervous system consists of two main parts – the central and peripheral nervous systems. The central nervous system (CNS) is the control center for the nervous system which receives, processes, interprets, and stores incoming sensory information. It consists of the brain and spinal cord. The peripheral nervous system consists of everything outside the brain and spinal cord. It handles the CNS’s input and output and divides into the somatic and autonomic nervous systems. The somatic nervous system allows for voluntary movement by controlling the skeletal muscles and it carries sensory information to the CNS. The autonomic nervous system regulates the functioning of blood vessels, glands, and internal organs such as the bladder, stomach, and heart. It consists of sympathetic and parasympathetic nervous systems. The sympathetic nervous system is involved when a person is intensely aroused. It provides the strength to fight back or to flee (fight-or-flight response). Eventually, the response brought about by the sympathetic nervous system must end so the parasympathetic nervous system kicks in to calm the body.
Figure 2.3. The Structure of the Nervous System
The Neuron
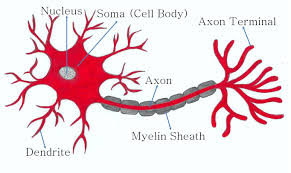
The fundamental unit of the nervous system is the neuron, or nerve cell (See Figure 2.4). It has several structures in common with all cells in the body. The nucleus is the control center of the body and the soma is the cell body. In terms of structures that make it different, these focus on the ability of a neuron to send and receive information. The axon sends signals/information through the neuron while the dendrites receive information from neighboring neurons and look like little trees. Notice the s on the end of dendrite and that axon has no such letter. In other words, there are lots of dendrites but only one axon. Also of importance to the neuron is the myelin sheath or the white, fatty covering which: 1) provides insulation so that signals from adjacent neurons do not affect one another and, 2) increases the speed at which signals are transmitted. The axon terminals are the end of the axon where the electrical impulse becomes a chemical message and is released into the synaptic cleft which is the space between neurons.
Though not neurons, glial cells play an important part in helping the nervous system to be the efficient machine that it is. Glial cells are support cells in the nervous system that serve five main functions.
- They act as a glue and hold the neuron in place.
- They form the myelin sheath.
- They provide nourishment for the cell.
- They remove waste products.
- They protect the neuron from harmful substances.
Finally, nerves are a group of axons bundled together like wires in an electrical cable.
Figure 2.4. The Structure of the Neuron
Neural Transmission
Transducers or receptor cells in the major organs of our five sensory systems – vision (the eyes), hearing (the ears), smell (the nose), touch (the skin), and taste (the tongue) – convert the physical energy that they detect or sense, and send it to the brain via the neural impulse. How so? We will cover this process in three parts.
Part 1. The Neural Impulse
- Step 1 – Neurons waiting to fire are said to be in resting potential and to be polarized (meaning they have a negative charge inside the neuron and a positive charge outside).
- Step 2 – If adequately stimulated, the neuron experiences an action potential and becomes depolarized. When this occurs, ion gated channels open allowing positively charged Sodium (Na) ions to enter. This shifts the polarity to positive on the inside and negative outside.
- Step 3 – Once the action potential passes from one segment of the axon to the next, the previous segment begins to repolarize. This occurs because the Na channels close and Potassium (K) channels open. K has a positive charge and so the neuron becomes negative again on the inside and positive on the outside.
- Step 4 – After the neuron fires, it will not fire again no matter how much stimulation it receives. This is called the absolute refractory period.
- Step 5 – After a short period of time, the neuron can fire again, but needs greater than normal levels of stimulation to do so. This is called the relative refractory period.
- Step 6 – Please note that the process is cyclical. Once the relative refractory period has passed the neuron returns to its resting potential.
Part 2. The Action Potential
Let’s look at the electrical portion of the process in another way and add some detail.
Figure 2.5. The Action Potential
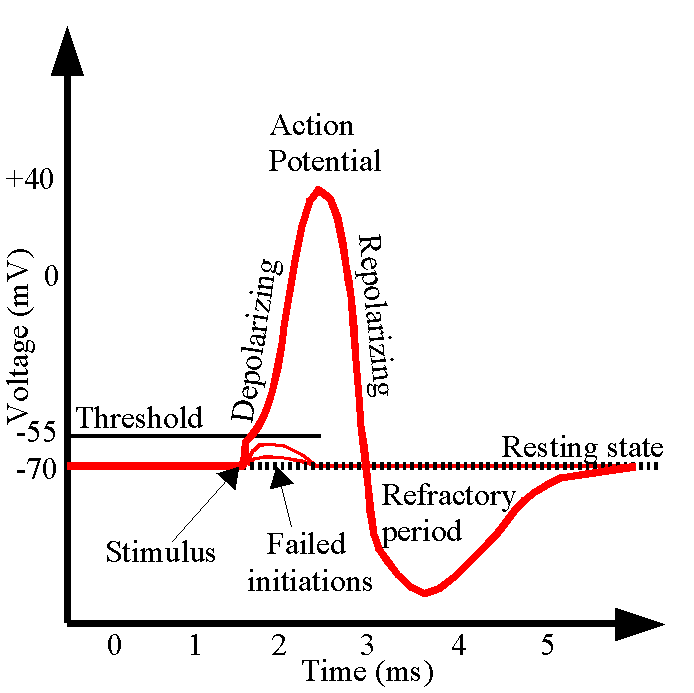
- Recall that a neuron is normally at resting potential and polarized. The charge inside is -70mV at rest.
- If it receives sufficient stimulation meaning that the polarity inside the neuron rises from -70 mV to -55mV defined as the threshold of excitation, the neuron will fire or send an electrical impulse down the length of the axon (the action potential or depolarization). It should be noted that it either hits -55mV and fires or it does not. This is the all-or-nothing principle. The threshold must be reached.
- Once the electrical impulse has passed from one segment of the axon to the next, the neuron begins the process of resetting called repolarization.
- During repolarization, the neuron will not fire no matter how much stimulation it receives. This is called absolute refractory period.
- The neuron next moves into relative refractory period meaning it can fire, but needs greater than normal levels of stimulation. Notice how the line has dropped below -70mV. Hence, to reach -55mV and fire, it will need more than the normal gain of +15mV (-70 to -55 mV).
- And then it returns to resting potential, as you saw in Figure 2.3
Ions are charged particles found both inside and outside the neuron. It is positively charged Sodium (Na) ions that cause the neuron to depolarize and fire and positively charged Potassium (K) ions that exit and return the neuron to a polarized state.
Part 3. The Synapse
The electrical portion of the neural impulse is just the start. The actual code passes from one neuron to another in a chemical form called a neurotransmitter. The point where this occurs is called the synapse. The synapse consists of three parts – the axon terminals of the sending neuron (presynaptic neuron); the space in between called the synaptic cleft, space, or gap; and the dendrite of the receiving neuron (postsynaptic neuron). Once the electrical impulse reaches the end of the axon, called the axon terminal, it stimulates synaptic vesicles or neurotransmitter sacs to release the neurotransmitter. Neurotransmitters will only bind to their specific receptor sites, much like a key will only fit into the lock it was designed for. You might say neurotransmitters are part of a lock-and-key system. What happens to the neurotransmitters that do not bind to a receptor site? They might go through reuptake which is a process in which the presynaptic neuron takes back excess neurotransmitters in the synaptic space for future use or enzymatic degradation when enzymes destroy excess neurotransmitters in the synaptic space.
Neurotransmitters
What exactly are some of the neurotransmitters which are so critical for neural transmission, and are important to our discussion of psychopathology?
- Dopamine – controls voluntary movements and is associated with the reward mechanism in the brain
- Serotonin – controls pain, sleep cycle, and digestion; leads to a stable mood and so low levels leads to depression
- Norepinephrine – increases the heart rate and blood pressure and regulates mood
- GABA – an inhibitory neurotransmitter responsible for blocking the signals of excitatory neurotransmitters responsible for anxiety and panic.
- Glutamate – an excitatory neurotransmitter associated with learning and memory
The critical thing to understand here is that there is a belief in the realm of mental health that chemical imbalances are responsible for many mental disorders. Chief among these are neurotransmitter imbalances. For instance, people with Seasonal Affective Disorder (SAD) have difficulty regulating serotonin. More on this throughout the book as we discuss each disorder.
The Brain
The central nervous system consists of the brain and spinal cord; the former we will discuss briefly and in terms of key structures which include:
- Medulla – regulates breathing, heart rate, and blood pressure
- Pons – acts as a bridge connecting the cerebellum and medulla and helps to transfer messages between different parts of the brain and spinal cord.
- Reticular formation – responsible for alertness and attention
- Cerebellum – involved in our sense of balance and for coordinating the body’s muscles so that movement is smooth and precise. Involved in the learning of certain kinds of simple responses and acquired reflexes.
- Thalamus – major sensory relay center for all senses except smell.
- Hypothalamus – involved in drives associated with the survival of both the individual and the species. It regulates temperature by triggering sweating or shivering and controls the complex operations of the autonomic nervous system
- Amygdala – responsible for evaluating sensory information and quickly determining its emotional importance
- Hippocampus – our “gateway” to memory. Allows us to form spatial memories so that we can accurately navigate through our environment and helps us to form new memories (involved in memory consolidation)
- The cerebrum has four distinct regions in each cerebral hemisphere. First, the frontal lobe contains the motor cortex which issues orders to the muscles of the body that produce voluntary movement. The frontal lobe is also involved in emotion and in the ability to make plans, think creatively, and take initiative. The parietal lobe contains the somatosensory cortex and receives information about pressure, pain, touch, and temperature from sense receptors in the skin, muscles, joints, internal organs, and taste buds. The occipital lobe contains the visual cortex and receives and processes visual information. Finally, the temporal lobe is involved in memory, perception, and emotion. It contains the auditory cortex which processes sound.
Figure 2.6. Anatomy of the Brain
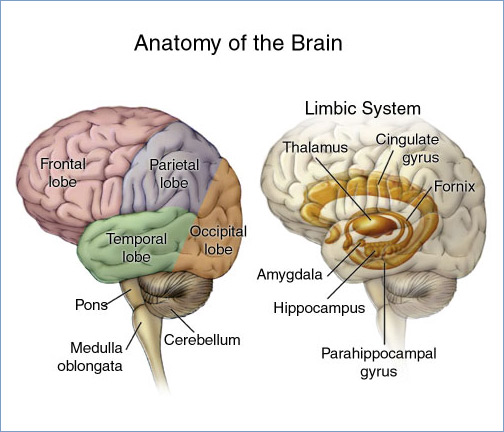
Of course, this is not an exhaustive list of structures found in the brain but gives you a pretty good idea of function and which structures help to support those functions. What is important to mental health professionals is that for some disorders, specific areas of the brain are involved. For instance, individuals with borderline personality disorder have been shown to have structural and functional changes in brain areas associated with impulse control and emotional regulation while imaging studies reveal differences in the frontal cortex and subcortical structures of individuals with OCD.
Exercises
Genes, Hormonal Imbalances, and Viral Infections
Genetic Issues and Explanations
DNA, or deoxyribonucleic acid, is our heredity material and is found in the nucleus of each cell packaged in threadlike structures known as chromosomes. Most of us have 23 pairs of chromosomes or 46 total. Twenty-two of these pairs are the same in both sexes, but the 23rd pair is called the sex chromosome and differs between males and females. Males have X and Y chromosomes while females have two Xs. According to the Genetics Home Reference website as part of NIH’s National Library of Medicine, a gene is “the basic physical and functional unit of heredity” (https://ghr.nlm.nih.gov/primer/basics/gene). They act as the instructions to make proteins and it is estimated by the Human Genome Project that we have between 20,000 and 25,000 genes. We all have two copies of each gene and one is inherited from our mother and one from our father.
Recent research has discovered that autism, ADHD, bipolar disorder, major depression, and schizophrenia all share genetic roots. They “were more likely to have suspect genetic variation at the same four chromosomal sites. These included risk versions of two genes that regulate the flow of calcium into cells.” For more on this development, please check out the article at: https://www.nih.gov/news-events/nih-research-matters/common-genetic-factors-found-5-mental-disorders. Likewise, twin and family studies have shown that people with first-degree relatives with OCD are at higher risk of developing the disorder themselves. The same is true of most mental disorders. Indeed, it is presently believed that genetic factors contribute to all mental disorders but typically account for less than half of the explanation. Moreover, most mental disorders are linked to abnormalities in many genes, rather than just one; that is, most are polygenetic.
Moreover, there are important gene-environment interactions that are unique for every person (even twins) which help to explain why some people with a genetic predisposition toward a certain disorder develop that disorder and others do not (e.g., why one identical twin may develop schizophrenia but the other does not). The diathesis-stress model posits that people can inherit tendencies or vulnerabilities to express certain traits, behaviors, or disorders, which may then be activated under certain environmental conditions like stress (e.g., abuse, traumatic events). However, it is also important to note that certain protective factors (like being raised in a consistent, loving, supportive environment) may modify the response to stress and thereby help to protect individuals against mental disorders.
Exercises
For more on the role of genes in the development of mental illness, check out this article from Psychology Today:
Hormonal Imbalances
The body has two coordinating and integrating systems in the body. The nervous system is one and the endocrine system is the second. The main difference between these two systems is in terms of the speed with which they act. The nervous system moves quickly with nerve impulses moving in a few hundredths of a second. The endocrine system moves slowly with hormones, released by endocrine glands, taking seconds, or even minutes, to reach their target. Hormones are important to psychologists because they organize the nervous system and body tissues at certain stages of development and activate behaviors such as alertness or sleepiness, sexual behavior, concentration, aggressiveness, reaction to stress, a desire for companionship.
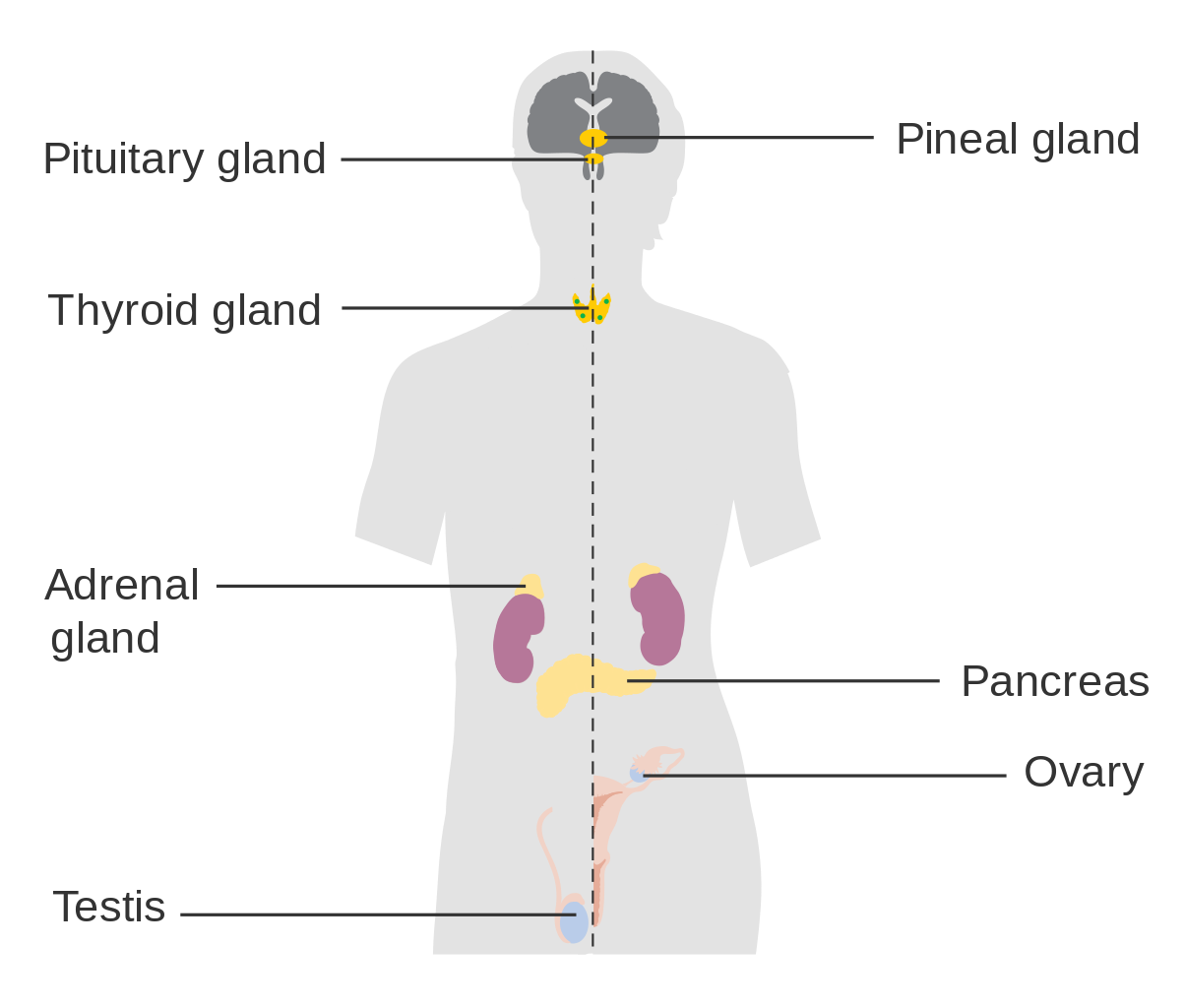
The pituitary gland is the “master gland” which regulates other endocrine glands. It influences blood pressure, thirst, contractions of the uterus during childbirth, milk production, sexual behavior and interest, body growth, the amount of water in the body’s cells, and other functions as well. The pineal gland produces melatonin which helps regulate the sleep-wake cycle and other circadian rhythms. Overproduction of the hormone melatonin can lead to Seasonal Affective Disorder (a specific type of Major Depressive Disorder). The thyroid gland produces thyroxin which facilitates energy, metabolism, and growth. Hypothyroidism is a condition in which the thyroid glands become underactive and this condition can produce symptoms of depression. In contrast, hyperthyroidism is a condition in which the thyroid glands become overactive and this condition can produce symptoms of mania. Therefore it is important for individuals experiencing these symptoms to have their thyroid checked, because conventional treatments for depression and mania will not correct the problem with the thyroid, and will therefore not resolve the symptoms. Rather, individuals with these conditions need to be treated with thyroid medications. Also of key importance to mental health professionals are the adrenal glands which are located on top of the kidneys, and release cortisol which helps the body deal with stress. However, chronically, elevated levels of cortisol can lead to increased weight gain, interfere with learning and memory, decrease the immune response, reduce bone density, increase cholesterol, and increase the risk of depression.
Figure 2.7. Hormone Systems
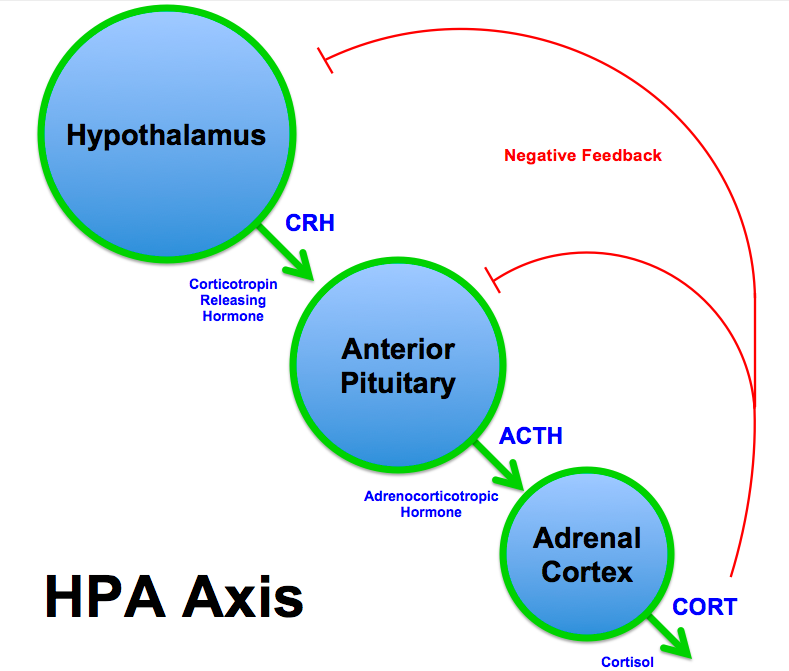
The Hypothalamic-Pituitary-Adrenal-Cortical Axis (HPA Axis) is the connection between the hypothalamus, pituitary glands, and adrenal glands. Specifically, the hypothalamus releases corticotropin-releasing factor (CRF) which stimulates the anterior pituitary to release adrenocorticotrophic hormone (ACTH), which in turn stimulates the adrenal cortex to release cortisol (see Figure 2.4). Malfunctioning of this system is implicated in a wide range of mental disorders including, depression, anxiety, and post-traumatic stress disorder. Exposure to chronic, unpredictable stress during early development can sensitive this system, making it over-responsive to stress (meaning it activates too readily and does not shut down appropriately). Sensitization of the HPA axis leads to an overproduction of cortisol which once again can damage the body and brain when it remains at chronically high levels.
Figure 2.8. The HPA Axis
For more on the link between cortisol and depression, check out this article:
Viral Infections
Infections can cause brain damage and lead to the development of mental illness or an exacerbation of symptoms. For example, evidence suggests that contracting strep infection can lead to the development of OCD, Tourette’s syndrome, and tic disorder in children (Mell, Davis, & Owens, 2005; Giedd et al., 2000; Allen et al., 1995; https://www.psychologytoday.com/blog/the-perfectionists-handbook/201202/can-infections-result-in-mental-illness). Influenza epidemics have also been linked to schizophrenia (Brown et al., 2004; McGrath and Castle, 1995; McGrath et al., 1994; O’Callaghan et al., 1991) though more recent research suggests this evidence is weak at best (Selten & Termorshuizen, 2017; Ebert & Kotler, 2005).
Treatments
Psychopharmacology and Psychotropic Drugs
One option to treat severe mental illness is psychotropic medications. These medications fall into five major categories. In this section we will broadly discuss these categories, and in the next we will cover them in more detail.
Antidepressants are used to treat depression, but also anxiety, insomnia, or pain. The most common types of antidepressants are selective serotonin reuptake inhibitors (SSRIs) and include Citalopram (Celexa), Paroxetine, and Fluoxetine (Prozac). They can often take 2-6 weeks to take effect. Possible side effects include weight gain, sleepiness, nausea and vomiting, panic attacks, or thoughts about suicide or dying.
Anti-anxiety medications help with the symptoms of anxiety and include the benzodiazepines such as Diazepam (Valium), Alprazolam (Xanax), and Lorazepam (Ativan). These medications are effective in reducing anxiety in the short-term and take less time to take effect than antidepressants which are also commonly prescribed for anxiety. However, benzodiazepines are rather addictive. As such, tolerance to these drugs can develop quickly and individuals may experience withdrawal symptoms (e.g., anxiety, panic, insomnia) when they cease taking the drugs. For this reason, benzodiazepines should not be used in the long-term. Side effects include drowsiness, dizziness, nausea, difficulty urinating, and irregular heartbeat, to name a few.
Stimulants increase one’s alertness and attention and are frequently used to treat ADHD. They include Lisdexamfetamine, the combination of dextroamphetamine and amphetamine, and Methylphenidate (Ritalin). Stimulants are generally effective and produce a calming effect. Possible side effects include loss of appetite, headache, motor tics or verbal tics, and personality changes such as appearing emotionless.
Antipsychotics are used to treat psychosis (i.e., hallucinations and delusions). They can also be used to treat eating disorders, severe depression, PTSD, OCD, ADHD, and Generalized Anxiety Disorder. Common antipsychotics include Chlorpromazine, Perphenazine, Quetiapine, and Lurasidone. Side effects include nausea, vomiting, blurred vision, weight gain, restlessness, tremors, and rigidity.
Mood stabilizers are used to treat bipolar disorder and at times depression, schizoaffective disorder, and disorders of impulse control. A common example is Lithium and side effects include loss of coordination, hallucinations, seizures, and frequent urination.
For more information on psychotropic medications, please visit:
https://www.nimh.nih.gov/health/topics/mental-health-medications/index.shtml
The use of these drugs has been generally beneficial to patients. Most report that their symptoms decline, leading them to feel better and improve their functioning. Also, long-term hospitalizations are less likely to occur as a result, though the medications do not benefit the individual in terms of improved living skills.
Electroconvulsive Therapy
According to Mental Health America, “Electroconvulsive therapy (ECT) is a procedure in which a brief application of electric stimulus is used to produce a generalized seizure.” Patients are placed on a padded bed and administered a muscle relaxant to avoid injury during the seizures. Annually, approximately 100,000 are treated using ECT for conditions including severe depression, acute mania, and suicidality. The procedure is still the most controversial available to mental health professionals due to “its effectiveness vs. the side effects, the objectivity of ECT experts, and the recent increase in ECT as a quick and easy solution, instead of long-term psychotherapy or hospitalization” (http://www.mentalhealthamerica.net/ect). Its popularity has declined since the 1940s and 1950s.
Psychosurgery
Another option to treat mental disorders is to perform brain surgeries. In the past, we have conducted trephining and lobotomies, neither of which are used today. Today’s techniques are much more sophisticated and have been used to treat schizophrenia, depression, and obsessive-compulsive disorder, though critics cite obvious ethical issues with conducting such surgeries as well as scientific issues. Due to these issues, psychosurgery is only used as a radical last resort when all other treatment options have failed to resolve a serious mental illness.
For more on psychosurgery, check out this article from Psychology Today:
https://www.psychologytoday.com/articles/199203/psychosurgery
Evaluation of the Model
The biological model is generally well respected today but suffers a few key issues. First, consider the list of side effects given for the psychotropic medications. You might make the case that some of the side effects are worse than the condition they are treating. Second, the viewpoint that all human behavior is explainable in biological terms, and therefore, when issues arise they can be treated using biological methods, overlooks factors that are not biological in nature. More on that over the next two sections.
References
Allen, A. J., Leonard, H. L., & Swedo, S. E. (1995). Case study: a new infection-triggered, autoimmune subtype of pediatric OCD and Tourette’s syndrome. Journal of the American Academy of Child & Adolescent Psychiatry, 34(3), 307-311.
Bridley, A., & Daffin, L. W. Jr. (2018). The Biological Model. In C. Cuttler (Ed), Essentials of Abnormal Psychology. Washington State University. Retrieved from https://opentext.wsu.edu/abnormalpsychology/.
Brown, A. S., Begg, M. D., Gravenstein, S., Schaefer, C. A., Wyatt, R. J., Bresnahan, M., … & Susser, E. S. (2004). Serologic evidence of prenatal influenza in the etiology of schizophrenia. Archives of general psychiatry, 61(8), 774-780.
Ebert, T., & Kotler, M. (2005). Prenatal exposure to influenza and the risk of subsequent development of schizophrenia. The Israel Medical Association Journal, 7(1), 35.
Giedd, J. N., Rapoport, J. L., Garvey, M. A., Perlmutter, S., & Swedo, S. E. (2000). MRI assessment of children with obsessive-compulsive disorder or tics associated with streptococcal infection. American Journal of Psychiatry, 157(2), 281-283.
McGrath, J. J., Pemberton, M. R., Welham, J. L., & Murray, R. M. (1994). Schizophrenia and the influenza epidemics of 1954, 1957 and 1959: A southern hemisphere study. Schizophrenia Research, 14(1), 1-8.
McGrath, J., & Castle, D. (1995). Does influenza cause schizophrenia? A five year review. Australian and New Zealand Journal of Psychiatry, 29(1), 23-31.
Mell, L. K., Davis, R. L., & Owens, D. (2005). Association between streptococcal infection and obsessive-compulsive disorder, Tourette’s syndrome, and tic disorder. Pediatrics, 116(1), 56-60.
O’Callaghan, E., Sham, P. C., Takei, N., Murray, R. M., & Glover, G. (1991). Schizophrenia after prenatal exposure to 1957 A2 influenza epidemic. The Lancet, 337(8752), 1248- 1250.
Selten, J. P., & Termorshuizen, F. (2017). The serological evidence for maternal influenza as risk factor for psychosis in offspring is insufficient: critical review and meta-analysis. Schizophrenia research, 183, 2-9.

