Personality Disorders
9.1 Personality Disorders
Cristina Crego; Thomas Widiger; Jorden A. Cummings; and Cailey Strauss
Section Learning Objectives
- Define what is meant by a personality disorder.
- Identify the five domains of general personality.
- Identify the six personality disorders proposed for retention in DSM-5.
- Summarize the etiology for antisocial and borderline personality disorder.
- Identify the treatment for borderline personality disorder.
Personality & the Five-Factor Model
Everybody has their own unique personality; that is, their characteristic manner of thinking, feeling, behaving, and relating to others (John, Robins, & Pervin, 2008). Some people are typically introverted, quiet, and withdrawn; whereas others are more extraverted, active, and outgoing. Some individuals are invariably conscientiousness, dutiful, and efficient; whereas others might be characteristically undependable and negligent. Some individuals are consistently anxious, self-conscious, and apprehensive; whereas others are routinely relaxed, self-assured, and unconcerned. Personality traits refer to these characteristic, routine ways of thinking, feeling, and relating to others. There are signs or indicators of these traits in childhood, but they become particularly evident when the person is an adult. Personality traits are integral to each person’s sense of self, as they involve what people value, how they think and feel about things, what they like to do, and, basically, what they are like most every day throughout much of their lives.
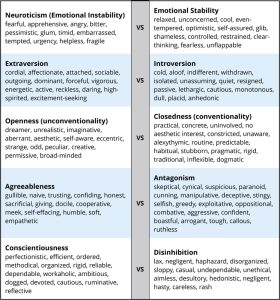
There are literally hundreds of different personality traits. All of these traits can be organized into the broad dimensions referred to as the Five-Factor Model (John, Naumann, & Soto, 2008). These five broad domains are inclusive; there does not appear to be any traits of personality that lie outside of the Five-Factor Model. This even applies to traits that you may use to describe yourself. Table 9.1 provides illustrative traits for both poles of the five domains of this model of personality. A number of the traits that you see in this table may describe you. If you can think of some other traits that describe yourself, you should be able to place them somewhere in this table.
DSM-5 Personality Disorders
When personality traits result in significant distress, social impairment, and/or occupational impairment, they are considered to be a personality disorder (American Psychiatric Association, 2013). The authoritative manual for what constitutes a personality disorder is provided by the American Psychiatric Association’s (APA) Diagnostic and Statistical Manual of Mental Disorders (DSM), the current version of which is DSM-5 (APA, 2013). The DSM provides a common language and standard criteria for the classification and diagnosis of mental disorders. This manual is used by clinicians, researchers, health insurance companies, and policymakers.
According to the DSM-V, a personality disorder is characterized by a pervasive, consistent, and enduring pattern of behaviour and internal experience that differs significantly from that which is usually expected in the individual’s culture. They typically have an onset in adolescence or early adulthood, persist over time, and cause distress or impairment. The pattern must be present in two or more of the four areas of cognition, emotion, interpersonal functioning, and impulse control. It must also not be better explained by another mental disorder or medical condition, or as the effects of a substance. There was much discussion in writing the DSM-V about changing the way in which personality disorders are diagnosed, but for now the system remains unchanged from the previous version of the DSM (the DSM-IV-TR). DSM-5 includes 10 personality disorders, grouped into three clusters: Cluster A (paranoid, schizoid, and schizotypal personality disorders), Cluster B (antisocial, borderline, histrionic, and narcissistic personality disorders), and Cluster C (avoidant, dependent, and obsessive-compulsive personality disorders).
This list of 10 though does not fully cover all of the different ways in which a personality can be maladaptive. DSM-5 also includes a “wastebasket” diagnosis of other specified personality disorder (OSPD) and unspecified personality disorder (UPD). This diagnosis is used when a clinician believes that a patient has a personality disorder but the traits that constitute this disorder are not well covered by one of the 10 existing diagnoses. OSPD and UPD or as they used to be referred to in previous editions – PDNOS (personality disorder not otherwise specified) are often one of the most frequently used diagnoses in clinical practice, suggesting that the current list of 10 is not adequately comprehensive (Widiger & Trull, 2007).
Each of the 10 DSM-5 (and DSM-IV-TR) personality disorders is a constellation of maladaptive personality traits, rather than just one particular personality trait (Lynam & Widiger, 2001). In this regard, personality disorders are “syndromes.” For example, avoidant personality disorder is a pervasive pattern of social inhibition, feelings of inadequacy, and hypersensitivity to negative evaluation (APA, 2013), which is a combination of traits from introversion (e.g., socially withdrawn, passive, and cautious) and neuroticism (e.g., self-consciousness, apprehensiveness, anxiousness, and worrisome). Dependent personality disorder includes submissiveness, clinging behavior, and fears of separation (APA, 2013), for the most part a combination of traits of neuroticism (anxious, uncertain, pessimistic, and helpless) and maladaptive agreeableness (e.g., gullible, guileless, meek, subservient, and self-effacing). Antisocial personality disorder is, for the most part, a combination of traits from antagonism (e.g., dishonest, manipulative, exploitative, callous, and merciless) and low conscientiousness (e.g., irresponsible, immoral, lax, hedonistic, and rash). See the 1967 movie, Bonnie and Clyde, starring Warren Beatty, for a nice portrayal of someone with antisocial personality disorder.
Some of the DSM-5 personality disorders are confined largely to traits within one of the basic domains of personality. For example, obsessive-compulsive personality disorder is largely a disorder of maladaptive conscientiousness, including such traits as workaholism, perfectionism, punctilious, ruminative, and dogged; schizoid is confined largely to traits of introversion (e.g., withdrawn, cold, isolated, placid, and anhedonic); borderline personality disorder is largely a disorder of neuroticism, including such traits as emotionally unstable, vulnerable, overwhelmed, rageful, depressive, and self-destructive (watch the 1987 movie, Fatal Attraction, starring Glenn Close, for a nice portrayal of this personality disorder); and histrionic personality disorder is largely a disorder of maladaptive extraversion, including such traits as attention-seeking, seductiveness, melodramatic emotionality, and strong attachment needs (see the 1951 film adaptation of Tennessee William’s play, Streetcar Named Desire, starring Vivian Leigh, for a nice portrayal of this personality disorder).
Due to the severity of symptoms (e.g., suicide), Canadian researchers have examined the rates of Cluster B personality disorders specifically (Cailhol et al., 2017). In Quebec, the 2011-2012 prevalence rates were 2.6% (lifetime) and 3.6% (12-month). Compared with the general provincial population, the mean years of lost life expectancy for men and women were 13 and 9 years, respectively (Cailhol et al., 2017).
It should be noted though that a complete description of each DSM-5 personality disorder would typically include at least some traits from other domains. For example, antisocial personality disorder (or psychopathy) also includes some traits from low neuroticism (e.g., fearlessness and glib charm) and extraversion (e.g., excitement-seeking and assertiveness); borderline includes some traits from antagonism (e.g., manipulative and oppositional) and low conscientiousness (e.g., rash); and histrionic includes some traits from antagonism (e.g., vanity) and low conscientiousness (e.g., impressionistic). Narcissistic personality disorder includes traits from neuroticism (e.g., reactive anger, reactive shame, and need for admiration), extraversion (e.g., exhibitionism and authoritativeness), antagonism (e.g., arrogance, entitlement, and lack of empathy), and conscientiousness (e.g., acclaim-seeking). Schizotypal personality disorder includes traits from neuroticism (e.g., social anxiousness and social discomfort), introversion (e.g., social withdrawal), unconventionality (e.g., odd, eccentric, peculiar, and aberrant ideas), and antagonism (e.g., suspiciousness).
The APA currently conceptualizes personality disorders as qualitatively distinct conditions; distinct from each other and from normal personality functioning. However, included within an appendix to DSM-5 is an alternative view that personality disorders are simply extreme and/or maladaptive variants of normal personality traits, as suggested herein. Nevertheless, many leading personality disorder researchers do not hold this view (e.g., Gunderson, 2010; Hopwood, 2011; Shedler et al., 2010). They suggest that there is something qualitatively unique about persons suffering from a personality disorder, usually understood as a form of pathology in sense of self and interpersonal relatedness that is considered to be distinct from personality traits (APA, 2012; Skodol, 2012). For example, it has been suggested that antisocial personality disorder includes impairments in identity (e.g., egocentrism), self-direction, empathy, and capacity for intimacy, which are said to be different from such traits as arrogance, impulsivity, and callousness (APA, 2012).
DSM-5 Description of Each Disorder
As mentioned, the DSM organizes personality disorders into 3 clusters.
Cluster A personality disorders involve odd and eccentric thinking or behaviour and include paranoid, schizoid, and schizotypal personality disorder. The Cluster B personality disorders involve dramatic, overly emotional, or unpredictable thinking or behaviour and include antisocial, borderline, histrionic, and narcissistic personality disorder. Cluster C personality disorders involve anxious, fearful thinking or behaviour and include avoidant, dependent, and obsessive-compulsive personality disorder.
Paranoid Personality Disorder
Paranoid personality disorder is characterized by a pattern of mistrust or suspiciousness of others. Their motives are generally interpreted as malicious. Even when no evidence supports this conclusion, individuals with this personality disorder tend to assume that others mean them harm. They may be suspicious of their close friends or family, and as a result tend to avoid confiding in others. There may also be a tendency to misinterpret harmless events or comments as threats. Individuals with paranoid personality disorder can carry persistent grudges or generally present as unforgiving of even minor slights. When feeling attacked or plotted against they are quick to react with anger and often lash out or plan to seek revenge. This personality disorder often involves an inability to trust one’s romantic partner, and even in the absence of any evidence to the contrary an individual may become convinced that their partner has been unfaithful. Interpersonally they often appear hostile, stubborn, sarcastic, rigid, controlling, and critical of others. However, it is important to note that members of minority groups may appear guarded or defensive in response to discrimination or neglect by the majority society. As with any personality disorder, cultural factors must not contribute to a diagnosis of paranoid personality disorder.
Schizoid Personality Disorder
If an individual generally remains detached from interpersonal relationships and has only a narrow range of emotional expression, they may be diagnosed with schizoid personality disorder. Someone with this disorder may derive no enjoyment from nor show any interest in close relationships including family, close friendships, or sexual relationships. They may choose solitary activities over interpersonal ones, find very few activities pleasurable or enjoyable, and may also seem indifferent when either praised or criticized by others. They may present as emotionally cold or distant and detached, with flattened affect. They may seem superficial or self-absorbed due to their disinterest in interpersonal relationships, and are generally not aware of (or do not respond to) social norms or cues. Individuals with schizoid personality disorder often find mechanical or abstract tasks (such as computer or mathematics) more attractive than social activities.
Schizotypal Personality Disorder
Schizotypal personality disorder is diagnosed when an individual is unable or unwilling to form close relationships and has cognitive or perceptual distortions or eccentric behaviour. These individuals may experience ideas of references and strange beliefs or “magical thinking” that influences how they behave and is inconsistent with cultural/societal norms. It is important to note that many cultural contexts or religious settings include beliefs in things that would otherwise be symptoms of schizotypal personality disorder, and this must be ruled out before a diagnosis can be made. People with this disorder may have unusual perceptions that include somatic illusions, and their speech and thinking may be “odd” (i.e., vague, metaphorical, overly detailed). Suspiciousness and paranoia are often present, as is inappropriate/constricted affect (i.e., appearing emotionally “stiff”), eccentric behaviour and appearance, and lack of close connections other than immediate family. Social anxiety is also common, but differs from Axis I anxiety disorders in that it does not decrease as one becomes more familiar with someone, and it is based in paranoia rather than fears of negative judgment.
Antisocial Personality Disorder
The diagnostic criteria for antisocial personality disorder specify that there must be a consistent pattern of disregarding or violating the rights of others since the age of 15. Specifically, this can involve unlawful behaviour or lying to or conning others for personal gain or pleasure. These individuals may be impulsive, irritable, aggressive, or reckless. As a result of these characteristics they may get into frequent physical fights or display a disregard for their own safety or that of others. They are frequently irresponsible and may fail to hold down a job or take care of financial obligations. Individuals with antisocial personality disorder often lack remorse, and as such they frequently present as indifferent to the suffering of others even when they have caused it. This personality disorder can only be diagnosed in someone 18 years or older, but conduct disorder must have been present prior to 15 years of age. There has been discussion about whether this diagnosis is disproportionately given to those from lower socioeconomic circumstances and care should be taken to tease apart survival strategies and traits from diagnosable symptoms of the disorder.
Borderline Personality Disorder
The hallmark of borderline personality disorder is a pervasive pattern of unstable interpersonal relationships, self-image, and emotions, with significant impulsivity. These individuals may respond to real or imagined abandonment by frantically trying to avoid it, and their relationships may be intense and unstable, and characterized by alternating between viewing someone as “all good” or “all bad.” They may have an extremely unstable sense of self which translates into frequently changing interests and goals, and their impulsivity may occur in areas such as finances, sexual behaviour, substance abuse, dangerous driving, or binge eating. Suicidal behaviour is common and can include gestures, threats, attempts, and self-mutilation. Their emotions are frequently labile (unstable and reactive), and their moods may last only a few hours or a few days. Many individuals with this disorder report feeling chronically “empty,” and they may struggle with intense and inappropriate anger that may be difficult for them to control. Borderline personality disorder may also cause paranoia or dissociation that comes and goes depending on stress levels. One must note that adolescents and younger adults who are undergoing identity issues may appear to have some of the symptoms of BPD. Also, BPD is disproportionately diagnosed in females (whereas antisocial PD is disproportionately diagnosed in men) and an argument has been made in the literature that perhaps the diagnosis unfairly pathologizes stereotypically female experiences or responses to trauma. Another discussion topic has been that the exact same symptoms in case studies are diagnosed by mental health professionals as symptoms of borderline personality disorder in females, but antisocial personality disorder in males.
Histrionic Personality Disorder
A diagnosis of histrionic personality disorder describes someone who may need to be the centre of attention in order to find a situation comfortable. They may interact with others in overly and inappropriately sexually seductive or provocative ways, and their emotions change quickly and tend to be quite shallow in expression. Their physical appearance is often used as a way of drawing attention to themselves, and their speech tends towards being overly vague and dramatic (for instance, making bold statements but having no details to back up their opinions). When these individuals express emotion it is often exaggerated and theatrical. They may also be easily influenced by others or circumstances and often consider their relationships to be more intimate and close than they actually are. Above all, individuals with histrionic personality disorder are known to show excessive emotion and seek attention to an extreme degree. Given that many of these traits are largely influenced by cultural context, the extent to which they cause significant impairment or distress must be evaluated before diagnosis can be made.
Narcissistic Personality Disorder
An individual with narcissistic personality disorder may have a grandiose sense of their own importance, which means that they may exaggerate their positive traits or successes and expect recognition). They may fantasize about success, power, beauty, brilliance, or love, and may see themselves as special and unique. This view of themselves may lead to a belief that they should only associate with other exceptional people. Someone with this disorder requires an excessive amount of admiration from others and feels entitled to special treatment. They may view others as needing to fulfill their needs and desires in a way that caters to their every whim. As such, these individuals sometimes take advantage of others in order to achieve their own goals and they may lack empathy or be unwilling or unable to recognize that others have valid thoughts, feelings, and needs. Although this disorder sometimes includes arrogant or haughty behaviour and attitudes, the individual may actually be envious of others. As a whole, this disorder involves extreme self-centred or self-absorbed behaviours and beliefs. Although ambition and confidence associated with this disorder may lead to significant vocational achievement, it may also cause impairment in functioning if an individual is unwilling to engage in tasks unless sure of success. They may also have difficulty working within a power structure that requires answering to someone with more power than themselves.
Avoidant Personality Disorder
Avoidant personality disorder generally involves an unwillingness to interact with people unless sure of being liked. This includes avoiding work that involves significant interaction or being restrained within relationships because of fearing criticism, rejection, disapproval, or shame. In fact, the individual is usually preoccupied with the idea of being criticized or rejected by others, and thus presents as inhibited when faced with new interpersonal relationships because of feeling inadequate. They may hold a view of themselves as socially inept, inferior, or unappealing. These individuals also tend to be quite reluctant to take any risks or try new activities because of an extreme fear of being embarrassed. What defines this personality disorder is the pattern of social inhibition, feelings of inadequacy or inferiority, and being hypersensitive to criticism. Unfortunately this disorder tends to create a vicious cycle, in which their fearful or tense presentation elicits negative responses from others, which in turn leads to more fear and avoidance. However, one must note that acculturation issues following immigration should not be confused with a diagnosis of avoidant personality disorder.
Dependent Personality Disorder
If someone shows a pattern of excessive neediness, clingy behaviour, submission, and fear of separation, they may be diagnosed with dependent personality disorder. This disorder may also include having difficulty making everyday decisions without seeking the input of others to an extreme degree. They may need others to take responsibility for large parts of their life, and may not be able to express dissenting opinions because of fearing disapproval or loss of support. Individuals with dependent personality disorder may have trouble starting projects or completing tasks on their own because they lack confidence in their abilities, and they may excessively try to secure nurturing support from others, even if it means they have to do things that they find unpleasant. This disorder also tends to involve feeling uncomfortable or helpless when left alone, due to feeling intense fear over having to take care of oneself. They may go from one relationship to another in order to avoid being left alone, as a result of being preoccupied with this fear. As with most other disorders, traits of dependent personality disorder can be heavily influenced by cultural factors. Being polite, deferent, and passive is highly regarded in some cultures and in order to be diagnosed with this disorder the individual’s behaviour must differ significantly from cultural norms.
Obsessive-Compulsive Personality Disorder
An individual with obsessive-compulsive personality disorder presents as preoccupied with details, rules, lists, order, organization, and schedules. This preoccupation is so intense that the main point of the activity being planned gets lost. Their perfectionism interferes with accomplishing goals, but they may also be so devoted to work and productivity that leisure time and friendships are sacrificed. These individuals may be extremely inflexible and scrupulous when it comes to issues of morals, ethics, or values (although this criterion must not be accounted for by religion or culture). They may find throwing out old or worthless items too difficult, even in the absence of sentimental value. This disorder also may make one hesitant to delegate or work cooperatively unless the workmate is willing to completely submit to how the individual feels the work should be done. In terms of finances, they may be extremely reluctant to spend money, choosing instead to hoard resources to prepare for an anticipated disaster in the future. These individuals also tend to present as extremely rigid and stubborn. Even normally “fun” activities may turn into structured tasks for someone with obsessive-compulsive personality disorder.
Validity
It is quite possible that in future revisions of the DSM some of the personality disorders included in DSM-5 will no longer be included. In fact, for DSM-5 it was originally proposed that four be deleted. The personality disorders that were slated for deletion were histrionic, schizoid, paranoid, and dependent (APA, 2012). The rationale for the proposed deletions was in large part because they are said to have less empirical support than the diagnoses that were at the time being retained (Skodol, 2012). There is agreement within the field with regard to the empirical support for the borderline, antisocial, and schizotypal personality disorders (Mullins-Sweat, Bernstein, & Widiger, 2012; Skodol, 2012). However, there is a difference of opinion with respect to the empirical support for the dependent personality disorder (Bornstein, 2012; Livesley, 2011; Miller, Widiger, & Campbell, 2010; Mullins-Sweat et al., 2012).
Little is known about the specific etiology for most of the DSM-5 personality disorders. Because each personality disorder represents a constellation of personality traits, the etiology for the syndrome will involve a complex interaction of an array of different neurobiological vulnerabilities and dispositions with a variety of environmental, psychosocial events. Antisocial personality disorder, for instance, is generally considered to be the result of an interaction of genetic dispositions for low anxiousness, aggressiveness, impulsivity, and/or callousness, with a tough, urban environment, inconsistent parenting, poor parental role modeling, and/or peer support (Hare, Neumann, & Widiger, 2012). Borderline personality disorder is generally considered to be the result of an interaction of a genetic disposition to negative affectivity interacting with a malevolent, abusive, and/or invalidating family environment (Hooley, Cole, & Gironde, 2012).
To the extent that one considers the DSM-5 personality disorders to be maladaptive variants of general personality structure, as described, for instance, within the Five-Factor Model, there would be a considerable body of research to support the validity for all of the personality disorders, including even the histrionic, schizoid, and paranoid. There is compelling multivariate behavior genetic support with respect to the precise structure of the Five-Factor Model (e.g., Yamagata et al., 2006), childhood antecedents (Caspi, Roberts, & Shiner, 2005), universality (Allik, 2005), temporal stability across the lifespan (Roberts & DelVecchio, 2000), ties with brain structure (DeYoung, Hirsh, Shane, Papademetris, Rajeevan, & Gray, 2010), and even molecular genetic support for neuroticism (Widiger, 2009).
Treatment
Personality disorders are relatively unique because they are often “ego-syntonic;” that is, most people are largely comfortable with their selves, with their characteristic manner of behaving, feeling, and relating to others. As a result, people rarely seek treatment for their antisocial, narcissistic, histrionic, paranoid, and/or schizoid personality disorder. People typically lack insight into the maladaptivity of their personality.

One clear exception though is borderline personality disorder (and perhaps as well avoidant personality disorder). Neuroticism is the domain of general personality structure that concerns inherent feelings of emotional pain and suffering, including feelings of distress, anxiety, depression, self-consciousness, helplessness, and vulnerability. Persons who have very high elevations on neuroticism (i.e., persons with borderline personality disorder) experience life as one of pain and suffering, and they will seek treatment to alleviate this severe emotional distress. People with avoidant personality may also seek treatment for their high levels of neuroticism (anxiousness and self-consciousness) and introversion (social isolation). In contrast, narcissistic individuals will rarely seek treatment to reduce their arrogance; paranoid persons rarely seek treatment to reduce their feelings of suspiciousness; and antisocial people rarely (or at least willfully) seek treatment to reduce their disposition for criminality, aggression, and irresponsibility.
Nevertheless, maladaptive personality traits will be evident in many individuals seeking treatment for other mental disorders, such as anxiety, mood, or substance use. Many of the people with a substance use disorder will have antisocial personality traits; many of the people with mood disorder will have borderline personality traits. The prevalence of personality disorders within clinical settings is estimated to be well above 50% (Torgersen, 2012). As many as 60% of inpatients within some clinical settings are diagnosed with borderline personality disorder (APA, 2000). Antisocial personality disorder may be diagnosed in as many as 50% of inmates within a correctional setting (Hare et al., 2012). It is estimated that 10% to 15% of the general population meets criteria for at least one of the 10 DSM-IV-TR personality disorders (Torgersen, 2012), and quite a few more individuals are likely to have maladaptive personality traits not covered by one of the 10 DSM-5 diagnoses.
The presence of a personality disorder will often have an impact on the treatment of other mental disorders, typically inhibiting or impairing responsivity. Antisocial persons will tend to be irresponsible and negligent; borderline persons can form intensely manipulative attachments to their therapists; paranoid patients will be unduly suspicious and accusatory; narcissistic patients can be dismissive and denigrating; and dependent patients can become overly attached to and feel helpless without their therapists.
It is a misnomer, though, to suggest that personality disorders cannot themselves be treated. Personality disorders are among the most difficult of disorders to treat because they involve well-established behaviors that can be integral to a client’s self-image (Millon, 2011). Nevertheless, much has been written on the treatment of personality disorder (e.g., Beck, Freeman, Davis, & Associates, 1990; Gunderson & Gabbard, 2000), and there is empirical support for clinically and socially meaningful changes in response to psychosocial and pharmacologic treatments (Perry & Bond, 2000). The development of an ideal or fully healthy personality structure is unlikely to occur through the course of treatment, but given the considerable social, public health, and personal costs associated with some of the personality disorders, such as the antisocial and borderline, even just moderate adjustments in personality functioning can represent quite significant and meaningful change.
Nevertheless, manualized and/or empirically validated treatment protocols have been developed for only one specific personality disorder, borderline (APA, 2001).
Focus Topic: Treatment of Borderline Personality Disorder
Dialectical behavior therapy (Lynch & Cuyper, 2012) and mentalization therapy (Bateman & Fonagy, 2012): Dialectical behavior therapy is a form of cognitive-behavior therapy that draws on principles from Zen Buddhism, dialectical philosophy, and behavioral science. The treatment has four components: individual therapy, group skills training, telephone coaching, and a therapist consultation team, and will typically last a full year. As such, it is a relatively expensive form of treatment, but research has indicated that its benefits far outweighs its costs, both financially and socially.
It is unclear why specific and explicit treatment manuals have not been developed for the other personality disorders. This may reflect a regrettable assumption that personality disorders are unresponsive to treatment. It may also reflect the complexity of their treatment. As noted earlier, each DSM-5 disorder is a heterogeneous constellation of maladaptive personality traits. In fact, a person can meet diagnostic criteria for the antisocial, borderline, schizoid, schizotypal, narcissistic, and avoidant personality disorders and yet have only one diagnostic criterion in common. For example, only five of nine features are necessary for the diagnosis of borderline personality disorder; therefore, two persons can meet criteria for this disorder and yet have only one feature in common. In addition, patients meeting diagnostic criteria for one personality disorder will often meet diagnostic criteria for another. This degree of diagnostic overlap and heterogeneity of membership hinders tremendously any effort to identify a specific etiology, pathology, or treatment for a respective personality disorder as there is so much variation within any particular group of patients sharing the same diagnosis (Smith & Zapolski, 2009).
Of course, this diagnostic overlap and complexity did not prevent researchers and clinicians from developing dialectical behavior therapy and mentalization therapy. A further reason for the weak progress in treatment development is that, as noted earlier, persons rarely seek treatment for their personality disorder. It would be difficult to obtain a sufficiently large group of people with, for instance, narcissistic or obsessive–compulsive disorder to participate in a treatment outcome study, one receiving the manualized treatment protocol, the other receiving treatment as usual.
Conclusions
It is evident that all individuals have a personality, as indicated by their characteristic way of thinking, feeling, behaving, and relating to others. For some people, these traits result in a considerable degree of distress and/or impairment, constituting a personality disorder. A considerable body of research has accumulated to help understand the etiology, pathology, and/or treatment for some personality disorders (i.e., antisocial, schizotypal, borderline, dependent, and narcissistic), but not so much for others (e.g., histrionic, schizoid, and paranoid). However, researchers and clinicians are now shifting toward a more dimensional understanding of personality disorders, wherein each is understood as a maladaptive variant of general personality structure, thereby bringing to bear all that is known about general personality functioning to an understanding of these maladaptive variants.
Outside Resources
Structured Clinical Interview for DSM-5 (SCID-5) https://www.appi.org/products/structured-clinical-interview-for-dsm-5-scid-5
Web: DSM-5 website discussion of personality disorders http://www.dsm5.org/ProposedRevision/Pages/PersonalityDisorders.aspx
Discussion Questions
- Do you think that any of the personality disorders, or some of their specific traits, are ever good or useful to have?
- If someone with a personality disorder commits a crime, what is the right way for society to respond? For example, does or should meeting diagnostic criteria for antisocial personality disorder mitigate (lower) a person’s responsibility for committing a crime?
- Given what you know about personality disorders and the traits that comprise each one, would you say there is any personality disorder that is likely to be diagnosed in one gender more than the other? Why or why not?
- Do you believe that personality disorders can be best understood as a constellation of maladaptive personality traits, or do you think that there is something more involved for individuals suffering from a personality disorder?
- The authors suggested Clyde Barrow as an example of antisocial personality disorder and Blanche Dubois for histrionic personality disorder. Can you think of a person from the media or literature who would have at least some of the traits of narcissistic personality disorder?
References
Allik, J. (2005). Personality dimensions across cultures. Journal of Personality Disorders, 19, 212–232.
American Psychiatric Association (2012). Rationale for the proposed changes to the personality disorders classification in DSM-5. Retrieved from http://www.dsm5.org/ProposedRevision/Pages/PersonalityDisorders.aspx.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5. Washington, D.C: American Psychiatric Association.
American Psychiatric Association. (2001). Practice guidelines for the treatment of patients with borderline personality disorder. Washington, DC: Author.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.) Washington, D.C: American Psychiatric Association.
Bateman, A. W., & Fonagy, P. (2012). Mentalization-based treatment of borderline personality disorder. In T. A. Widiger (Ed.), The Oxford handbook of personality disorders (pp. 767–784). New York, NY: Oxford University Press.
Beck, A. T., Freeman, A., Davis, D., and Associates (1990). Cognitive therapy of personality disorders, (2nd ed.). New York, NY: Guilford Press.
Bornstein, R. F. (2012). Illuminating a neglected clinical issue: Societal costs of interpersonal dependency and dependent personality disorder. Journal of Clinical Psychology, 68, 766–781.
Cailhol, L., Pelletier, E., Rochette, L., Laporte, L., David, P., Villeneuve, E., … & Lesage, A. (2017). Prevalence, mortality, and health care use among patients with Cluster B personality disorders clinical diagnosed in Quebec: A provincial cohort study, 2001-2012. The Canadian Journal of Psychiatry, 62, 336-342. doi: 10.1177/0706743717700818
Caspi, A., Roberts, B. W., & Shiner, R. L. (2005). Personality development: Stability and change. Annual Review of Psychology, 56, 453–484.
Crego, C. & Widiger, T. (2020). Personality Disorders. In R. Biswas-Diener & E. Diener (Eds), Noba textbook series: Psychology. Champaign, IL: DEF publishers. Retrieved from http://noba.to/67mvg5r2.
DeYoung, C. G., Hirsh, J. B., Shane, M. S., Papademetris, X., Rajeevan, N., & Gray, J. (2010). Testing predictions from personality neuroscience: Brain structure and the Big Five. Psychological Science, 21, 820–828.
Gunderson, J. G. (2010). Commentary on “Personality traits and the classification of mental disorders: Toward a more complete integration in DSM-5 and an empirical model of psychopathology.” Personality Disorders: Theory, Research, and Treatment, 1, 119–122.
Gunderson, J. G., & Gabbard, G. O. (Eds.), (2000). Psychotherapy for personality disorders. Washington, DC: American Psychiatric Press.
Hare, R. D., Neumann, C. S., & Widiger, T. A. (2012). Psychopathy. In T. A. Widiger (Ed.), The Oxford handbook of personality disorders (pp. 478–504). New York, NY: Oxford University Press.
Hooley, J. M., Cole, S. H., & Gironde, S. (2012). Borderline personality disorder. In T. A. Widiger (Ed.), The Oxford handbook of personality disorders (pp. 409–436). New York, NY: Oxford University Press.
Hopwood, C. J. (2011). Personality traits in the DSM-5. Journal of Personality Assessment, 93, 398–405.
John, O. P., Naumann, L. P., & Soto, C. J. (2008). Paradigm shift to the integrative Big Five trait taxonomy: History, measurement, and conceptual issues. In O. P. John, R. R. Robins, & L. A. Pervin (Eds.), Handbook of personality. Theory and research (3rd ed., pp. 114–158). New York, NY: Guilford Press.
John, O. P., Robins, R. W., & Pervin, L. A. (Eds.), (2008). Handbook of personality. Theory and Research (3rd ed.). New York, NY: Guilford Press.
Livesley, W. J. (2011). Confusion and incoherence in the classification of personality disorder: Commentary on the preliminary proposals for DSM-5. Psychological Injury and Law, 3, 304–313.
Lynam, D. R., & Widiger, T. A. (2001). Using the five factor model to represent the DSM-IV personality disorders: An expert consensus approach. Journal of Abnormal Psychology, 110, 401–412.
Lynch, T. R., & Cuper, P. F. (2012). Dialectical behavior therapy of borderline and other personality disorders. In T. A. Widiger (Ed.), The Oxford handbook of personality disorders (pp. 785–793). New York, NY: Oxford University Press.
Miller, J. D., Widiger, T. A., & Campbell, W. K. (2010). Narcissistic personality disorder and the DSM-V. Journal of Abnormal Psychology, 119, 640–649.
Millon, T. (2011). Disorders of personality. Introducing a DSM/ICD spectrum from normal to abnormal (3rd ed.). New York, NY: John Wiley & Sons.
Mullins-Sweatt; Bernstein; Widiger. Retention or deletion of personality disorder diagnoses for DSM-5: an expert consensus approach. Journal of personality disorders 2012;26(5):689-703.
Perry, J. C., & Bond, M. (2000). Empirical studies of psychotherapy for personality disorders. In J. Gunderson and G. Gabbard (Eds.), Psychotherapy for personality disorders (pp. 1–31). Washington DC: American Psychiatric Press.
Roberts, B. W., & DelVecchio, W. F. (2000). The rank-order consistency of personality traits from childhood to old age: A quantitative review of longitudinal studies. Psychological Bulletin, 126, 3–25.
Shedler, J., Beck, A., Fonagy, P., Gabbard, G. O., Gunderson, J. G., Kernberg, O., … Westen, D. (2010). Personality disorders in DSM-5. American Journal of Psychiatry, 167, 1027–1028.
Skodol, A. (2012). Personality disorders in DSM-5. Annual Review of Clinical Psychology, 8, 317–344.
Smith, G. G., & Zapolski, T. C. B. (2009). Construct validation of personality measures. In J. N. Butcher (Ed.), The Oxford Handbook of Personality Assessment (pp. 81–98). New York, NY: Oxford University Press.
Torgerson, S. (2012). Epidemiology. In T. A. Widiger (Ed.), The Oxford handbook of personality disorders (pp. 186–205). New York, NY: Oxford University Press.
Widiger, T. A. (2009). Neuroticism. In M. R. Leary and R.H. Hoyle (Eds.), Handbook of individual differences in social behavior (pp. 129–146). New York, NY: Guilford Press.
Widiger, T. A., & Trull, T. J. (2007). Plate tectonics in the classification of personality disorder: Shifting to a dimensional model. American Psychologist, 62, 71–83.
Yamagata, S., Suzuki, A., Ando, J., One, Y., Kijima, N., Yoshimura, K., … Jang, K. L. (2006). Is the genetic structure of human personality universal? A cross-cultural twin study from North America, Europe, and Asia. Journal of Personality and Social Psychology, 90, 987–998.

